Purpose
1- Embryological and anatomical remember
2- Sequences and suitableplanes for MR study
3- Pathology
Methods and Materials
The most common reaction of the pericardium against any aggression is the fluid production.
Other more infrequent reactions are thickening of their layers,
calcification,
nodules or masses.
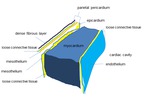
1.- ANATOMY Fig.1
The pericardium is an anatomically simple structure that can be affected by multiple processes.
- The outer layer it is fibrous pericardium,
hard and fibrous,
that binds to the adyacent structures that anchor the heart:
Joins the central tendon of the diaphragm by the pericardiophrenic ligament.
Fig.
2
On the front face it is inserted...
Results
CT and MR imaging should be used when findings at echocardiography are difficult to interpret or conflict with clinical findings.
Infection,
neoplasm,
injury,
and congenital disease all may affect the pericardium.
Although echocardiography is the primary imaging modality used to examine the pericardium,
CT and MR imaging provide various advantages,
especially in cases of loculated or hemorrhagic effusion,
constrictive pericarditis,
and pericardial masses.
Conclusion
It is mandatory for the radiologist to know the normal anatomy,variants and the pathologic processes that may affect the pericardium and the MR protocols used to accurately study the pericardium.
MRI can study the whole pericardium to show its morphology and approximate its histology by evaluation of the signal intensity.
MRI offers a correct assessment of pericardial effusion,distribution,
presence of loculations and content.
MRI offers a functional assessment of the impact of the pericardial disease
MRI is essential in cases the echocardiographic information is insufficient,...
References
Review.
Cardiac Masses,
Part 2: Key Imaging Features for Diagnosis and Surgical Planning.
Orla Buckley,
Rachna Madan,
Raymond Kwong,
Frank J.
Rybicki,
Andetta Hunsaker.
American Journal of Roentgenology.
2011;197:W842-W851.
10.2214/AJR.11.6903
Pictorial Essay.
MRI of Cardiomyopathy.Elena Belloni,
Francesco De Cobelli,
Antonio Esposito,
Renata Mellone,
Gianluca Perseghin,Tamara Canu,
Alessandro Del MaschioAmerican Journal of Roentgenology.
2008;191:1702-1710.
10.2214/AJR.07.3997
Review.
Cardiac Masses,
Part 1: Imaging Strategies and Technical Considerations.
Orla Buckley,
Rachna Madan,
Raymond Kwong,
Frank J.
Rybicki,
Andetta Hunsaker.
American Journal of Roentgenology.
2011;197:W837-W841.
10.2214/AJR.10.7260
Review.
MRI of Hypertrophic...