Purpose
Thermal ablation has been used for a number of years in the treatment of both primary and secondary malignancies,
mainly in the liver and lung.
There is growing evidence to support its use,
and the Royal College of Radiology predicts that it will have a more important role in the future.
The technique is recognised by NICE (1) who acknowledge that further research is required to fully define its exact role.
Because of the difficulty in performing true randomised controlled studies,
much of the supportive...
Methods and materials
90 tumours in 45 patients treated with radiofrequency ablation (RFA) between April 2009 and August 2013 during 83 separate procedures were analysed using a prospective database
All procedures were performed under deep conscious sedation (intravenous morphine and midazolam) using pulse oximetry and real time Bispectral Index (BIS) monitoring (Aspect Medical Systems,
Inc.
Norwood,
MA,
USA).
Patients were positioned depending upon the location of the lesion.
Local anaesthetic (20ml 1% lignocaine) was infiltrated to the pleura under CT guidance.
Ablation was performed using either the Boston...
Results
Survival
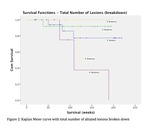
Median survival was 105 weeks,
with 1 year,
2 year and 3-year survival 95.5%,
89.9% and 77.7% respectively.
Patients who had a total number of tumour lesions ≥ 3 ablated were found to have a mean survival of 150 weeks,
compared to 195 weeks in those with a total number of lesions ≤ 2.
This almost reached statistical significance (p=0.091) (figures 1 and 2).
The following variables were not statistically significant (table 1): mean maximum tumour size; initial number of tumours ablated; whether the...
Conclusion
Pulmonary RFA is a safe and well-tolerated technique.
Compared with surgical resection RFA is less invasive and may be performed under conscious sedation,
either as a day case or with a single night in hospital,
with negligible effect on the patient’s lung function.
When selecting patients for surgical metastatectomy performance status and poor lung function can preclude some patients from surgical treatment (2),
whereas this is less likely to preclude patients from treatment with RFA.
The 3-year survival from our data was 77.7% for pulmonary...
Personal information
1.
Dr Christopher Zagorski,
Department of Radiology
Norfolk and Norwich University Hospital,
Norfolk,
NR4 7UY,
01603 286286
2.
Dr Stuart Forbes,
Department of Surgery,
Ipswich Hospital,
Heath Road,
Ipswich,
Suffolk,
IP4 5PD,
01473 712233
3.
Dr Paul Jennings,
Department of Radiology
Ipswich Hospital,
Heath Road,
Ipswich,
Suffolk,
IP4 5PD,
01473 712233
4.
Dr Rubin Soomal,
Department of Oncology
Ipswich Hospital,
Heath Road,
Ipswich,
Suffolk,
IP4 5PD,
01473 712233
5.
Dr Simon Smith,
Supervising author/author for correspondence
Department of Radiology
Ipswich Hospital,
Heath Road,
Ipswich,
Suffolk,...
References
1.
National Institute for Health and Clinical.
IPG372 Percutaneous radiofrequency ablation for primary or secondary lung cancers: guidance.
NHS ,
2010.
2. Davidson R,
Nwogu C,
Brentjens M,
et al.
The surgical management of pulmonary metastases: Current concepts.
Vol.
10.
Surg Oncol,
2001.
3.
Gillams A,
Khan Z,
Osborn P et al.
Survival after Radiofrquency Ablation in 122 patients with inoperable colorectal lung metastases.
Vol.
36.
Cardiovasc Intervent Radiol,
n.d.
4.
Yan TD,
King J,
Sjarif A et al.
Percutaneous radiofrequency ablation of pulmonary metastases...