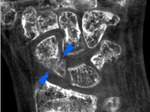
Received CBCT-images of distal segments of upper and lower extremities were distinguished by high-resolution with a detailed mapping of bone structure: accurate differentiation and direction of bone trabeculae.
It became possible to measure a thickness of cortical bone,
even if it was less than 1 mm.
During the comparative analysis it was found that visualization of bone structure on CBCT-images was comparable or even exceeded MSCT and digital microfocus X-ray images,
but it was not defined reliable on standard X-ray images.
In addition,
small bone fragments and areas of pathological alteration of bone tissue (even under 1 – 2 mm) were observed reliably on CBCT-images.
It became possible to specify its localization and spatial location (Fig.
3,
4).
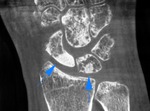
The signs of different kinds of fractures in 42,7 % (n = 41) cases were visualized reliably on CBCT with subsequent building of multiplanar and 3D-reconstructions.
Osteoreparation abnormality process (false joints,
neoarthrosis,
avascular necrosis) was detected in 18,8 % (n = 18) cases.
The absence of the callus,
smoothing and curving of bone fragments and detection of closing plates at the level of the edges of fragments in the presence of false joints and signs of avascular necrosis as areas of osteosclerotic changes with a loss of trabecular structure,
surrounded by a rim of sclerosis,
were revealed convincing on MSCT and CBCT.
It was not always possible to establish the presence of the closing plates at the level of the edges of fragments or the signs of avascular necrosis by SR (Fig.
5–8).
Our attention was attracted by the lack of significant artifacts from different kinds of massive metal constructions,
foreign bodies with metal density and cell employ bandages on CBCT-images as distinct from MSCT (Fig.
9,
A–E).
CBCT-images of distal extremities were characterized by high spatial resolution,
optimal signal-to-noise ratio,
uniform accuracy and dynamic range grayscale,
which allowed estimating not only of bone structure,
but dense soft tissue formations as well: capsule-ligamentous apparatus,
tendons,
palmar and plantar aponeurosis,
clusters of excess fluid accumulation in sinovitis and tendovaginitis (Fig.
10,
A,
B).
These CBCT-findings were comparable with MSCT,
but were not always convincing by SR and DMFR.
We also managed to determine reliably the presence of the tofuses on CBCT-images of patients with podagric arthropaty in 27,1 % (n = 26) cases.
It became possible to ascertain its size,
localization,
spatial location and to assess the relationships with the surrounding tissues (Fig.
11,
12).
CBCT-visualization of crystals of uric acid accumulation was comparable with MSCT and DMFR,
but was not always convincing by SR.
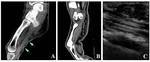
In 22,9 % (n = 22) cases signs of palmar,
palmar-finger forms of Dupuytren's contracture and of plantar aponeurosis degeneration were detected.
Funnel-shaped retraction of skin on a palm or a foot surface,
restriction of extension of one or more fingers on the level of changes,
as well,
associated with degeneration of one or more beams of aponeurosis defined with external inspection.
During comparative analysis of MSCT,
MRI,
US and CBCT-images we noted the signs of fibrous degeneration of palmar or plantar aponeurosis as a limited retraction of the skin under it.
A thickened connective tissue cords have been visualized reliably between skin and aponeurosis,
an edge between them differentiated separately not always.
A significant thickening of the aponeurosis with a heterogeneous structure and illegible,
uneven outline subcutaneously at this level has been determined.
A modified aponeurosis was commissured with tendon and skin depending on the stage or form of the contracture in a varying degree.
There were initial signs or symptoms of a severe deformity of the tendon on this background.
Moreover,
all the above-listed studies (MSCT,
MRI,
US and CBCT) of patients with signs of aponeurosis degeneration revealed the presence of tenosinovitis of flexor fingers and degenerative-dystrophic changes in bones of distal segments of involved extremities (Fig.
13,
A–C). An assessment of SR of distal extremities didn't not allowed us to obtain any data about palmar or plantar aponeurosis of such patients.