Anterior and posterior normal urethra on RUG and VUG: different methods - different appearance
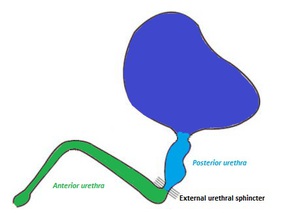
To understand urethrography images and the differences in the appearance of anterior of posterior urethra depending on the type of the urethrography performed,
one should consider the presence of the external urethral sphincter at the urogenital diaphragm.
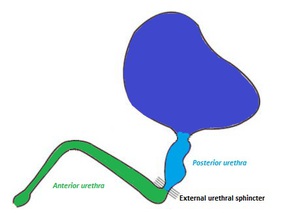
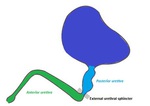
Fig. 2: The location of the internal urethral sphincter in association with the anterior and posterior male urethra.
References: John G. Gearhart, Richard C. Rink, Pierre D. E. Mouriquan. Pediatric Urology, 2nd ed. Elsevier Health Sciences, 2009
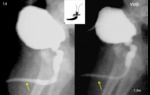
The resistance that the external urethral sphincter exerts to the retrograde (ascending) injection of contrast in Retrograde Urethrography (RUG) creates full distension and therefore better depiction of the anterior urethra.
In a similar manner,
the resistance that is exerted at the same level of the external urethral sphincter to the descending flow of contrast during micturition explains the better dilatation of the posterior urethra in Voiding Urethrography (VUG).
The posterior urethra in RUG may be minimally opacified,
depicted as a thin linear structure,
because contrast flows unimpeded into the bladder.
Contrast flow may even stop at the level of the urogenital diaphragm and posterior urethra may not be shown at all.
These imaging findings should never be mistaken for pathology and each part of the urethra should be appreciated by the appropriate urethrogram and when possible by both examinations.
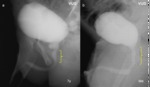
Retrograde urethrography (RUG) evaluates better the anterior,
while voiding urethrography (VUG) the posterior urethra. Fig. 3
Normal imaging findings in classic fluoroscopic urethrography
In classic urethrography male urethra is seen as a smooth tubular structure,
shaped like a horizontally inverted “S” (when penis is not erect) suspended by the urogenital diaphragm and the suspensory ligament.

Fig. 4: In urethrography male urethra is shaped like a horizontally inverted “S”.
The posterior urethra
Prostatic urethra
The prostatic part of the urethra begins at the vesical neck and internal sphincter,
courses through the prostatic gland and ends at the urogenital diaphragm.
It is approximately 3-4cm long,
has a crescent shape and is the widest and most distensible part of the male urethra measuring 1- 1,5cm. Fig. 5
There are several urethral and paraurethral structures that can be indirectly depicted in the prostatic part of the urethra on an urethrogram,
such as:
- the verumontanum (seminal colliculus),
a prominence of the prostatic crest,
that produces an oval filling defect at the middle of the posterior prostatic wall (approximately 1-2cm long) Fig. 6
- the intermuscular incisura,
a muscular ridge,
that creates an indentation at the anterior wall of the prostatic urethra at the level of the verumontanum and can be mistaken for urethral valves Fig. 7
- the plica collicularis,
two linear fins of mucosa on the floor of the posterior urethra located caudally to the verumontanum,
that appear as thin,
non-obstructing indentations at the urethrogram and may encircle the urethra thus mimicking posterior urethral valves Fig. 8
- the prostatic utricle,
a remnant of the Müllerian duct,
is an anatomic variant that may occasionally fill with contrast during urethrography,
creating a small diverticulum at the posterior aspect of the prostatic urethra at the apex of the verumontanum Fig. 9
- the prostatic and ejaculatory ducts,
that open along the verumontanum,
may rarely be depicted by contrast material refluxing into them Fig. 19
Membranous urethra
Beginning from the apex of the prostate gland,
the membranous urethra traverses the urogenital diaphragm,
which contains the external urethral sphincter and pair of Cowper’s glands on each side.
It is the shortest (1-2cm) and the narrowest part of the male urethra with a maximum width of 5-7mm during voiding.
It is also the most fixed and thus the least distensible part of the urethra in fluoroscopic imaging studies. Fig. 10
The membranous urethra lies specifically between two radiologic landmarks: the distal end of the verumontanum (proximally) and the conical end of the bulbar urethra (distally). Fig. 11
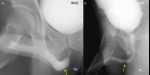
In VUG it appears as reduced urethral lumen distally to the prostatic urethra,
while in RUG as a thin,
opaque line continuing cephalad from the conical tip of the bulbous urethra.
Since it is located more proximal to the external sphincter,
it is depicted with a widest lumen in VUG than in RUG studies,
but regardless of the type of urethrography performed it remains the narrowest of the four parts of the male urethra.
The urogenital diaphragm and the external sphincter usually produce a circumferential narrowing of the urethral lumen,
marking the location of the membranous urethra. Fig. 11
The anterior urethra
Bulbous and penile (or pendulous) urethras
The bulbous urethra extends from the inferior margin of the urogenital diaphragm to the penoscrotal junction and the penile urethra extends from this junction to the external urethral meatus.
The anterior urethra is the longest of the urethral parts (14–15 cm),
surrounded by the corpus spongiosum penis.
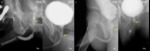
RUG shows the anterior urethra as a long,
wide lumen that tapers smoothly to a conical end at the level of the external urethral sphincter marking the bulbomembranous junction. In VUG studies the bulbar urethra has a less conical appearance and the anterior urethral lumen appears narrower than in RUG studies (6 mm). Fig. 12
The penoscrotal junction can be identified on urethrograms by a mild angulation caused by the suspensory ligament.
Depending on the tone of the ligament,
the positioning of the patient and the degree of traction of patient’s penis along the thigh during RUG,
the anterior urethra has a more or less elongated shape. Fig. 12
Its width is rather uniform at its whole length except from two normal dilatations:
- the “sump” of the bulbous urethra (called also bulb of the urethra or intrabulbar fossa) located at the proximal bulbous urethra,
where the urethral lumen is the widest
- the fossa navicularis at the distal penile urethra within the glans penis (1-1,5 cmlong). Fig. 13
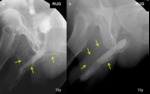
The bulbospongiosus (or bulbocavernosus) muscle may produce a false image of stenosis of the whole anterior urethra at VUG when the whole muscle contracts that usually quickly resolves. Fig. 14
A musculotendinous sling of the bulbocavernous muscle called constrictor nudae muscle,creates a mild indentation at the bulbous urethra at the urethrogram,
when contracted,
that should not be confused with a stricture. Fig. 15
Parallel to the course of the anterior urethra the periurethral glands of Littré are distributed,
most of which are located around the fossa navicularis and the urethral sump. When there is forceful injection of contrast material in RUG or more commonly when strictures or chronic inflammation are present, reflux of contrast into ducts of these glands or veins of the corpus spongiosum may be depicted. Fig. 16 Fig. 19
At the bulbous urethra drain also the Cowper’s glands ducts,
that may infrequently opacify as well,
appearing as a tubular structure extending proximally from the ventral surface of the bulbar urethra toward the urogenital diaphragm. Fig. 19
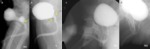
During VUG in uncircumcised patients,
contrast material may accumulate between the glans penis and the prepuce. Fig. 17
Differences in urethrograms regarding age
Urethrograms in boys and adults do not differ as far as radiologic anatomy is concerned.
Howerver,
there are differences concerning caliber and length of the male urethra between different age groups and between individuals,
especially regarding the penile urethra part and the prostatic part in men with benign prostatic hyperplasia.
Some variants may be found more frequently in children than in adults,
such as indentations from plica collicula,
the intermuscular incisura and the internal urethral sphincter. Fig. 18