1.
OVARIAN TORSION
Ovarian torsion is defined as partial or complete rotation of the ovarian vascular pedicle causing obstruction to venous outflow and arterial inflow. When fallopian tube also twists with the ovary,
it is known as adnexal torsion. Torsion of the ovarian blood supply will result in venous congestion,
hemorrhage,
and eventually ischemia.
Prolonged ischemia of the ovary or other adnexal structures can lead to necrosis,
resulting in loss of ovarian function or infection and peritonitis.
Torsion is reportedly more common on the right side (3:2).
This is possibly due to either the sigmoid colon on the left limiting movement or a hypermobile cecum on the right that is more permissive to movement.
In pediatric patients,
ovarian torsion can be caused by a variety of anatomic mechanisms. Most cases of torsion occur in ovaries containing masses,
such as functional cysts and neoplasms,
but also may occur with anatomically normal ovaries.
Proposed mechanisms that may increase the risk of ovarian torsion in a normal ovary include:
- Disproportionately elongated utero-ovarian ligament that allows excessive ovarian movements.
- Jarring movements of a relatively large ovary in a small infant.
- Associated Müllerian anomalies.
Ovarian torsion is an emergency that mandates early diagnosis and timely surgical exploration and detorsion to avoid the catastrophic consequence of further adnexal injury.
However,
because the signs and symptoms can mimic other acute abdominal conditions,
the preoperative diagnosis it is usually delayed.
On ultrasound,
this is typically seen as an increase in ovarian size where the central stroma has increased echogenicity and non-ovulatory follicles are pushed to the periphery.
An underlying ovarian lesion may be seen (possible lead point for torsion).
As torsion progresses,
the arterial supply is occluded and haemorrhagic infarction occurs with the development of hypoechogenic regions within the ovary.
Free pelvic fluid may be seen in >80% of cases.
Doppler ultrasound demonstrates absence of blood flow to the torted ovary.
The characteristic "whirlpool sign" may be seen on colour Doppler where the twisted vascular pedicle gives a corkscrew appearance.
However,
due to the dual ovarian blood supply (ovarian artery and ovarian branch of the uterine artery),
high-grade torsion is required to completely occlude arterial supply and therefore the presence of colour Doppler flow within an ovary does not exclude the diagnosis of torsion.
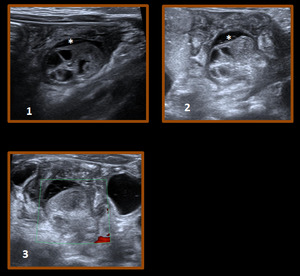
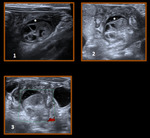
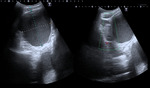
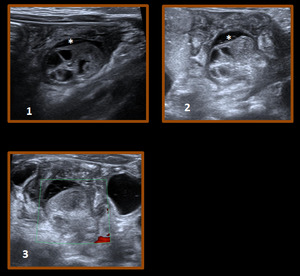
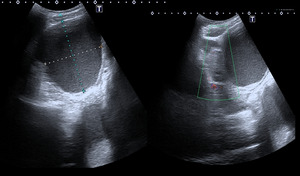
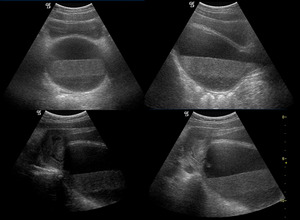
Fig. 2: 2-month-old girl with crying and paleness who referred us with suspicion of intestinal intussusception.
Fig. 1-2.An enlarged right ovary (25 mm) and hyperechogenic with multiple follicles are observed. Free liquid around the ovary (*).
Fig.3. No arterial or venous flow. No underlying ovarian lesion was found.
The diagnosis was ovarian torsion. The baby was operated on urgently and the ovary was distorsioned, although it already had areas of ischemia.
References: Department of Radiology, Hospital Universitario Marqués de Valdecilla - Santander/ES
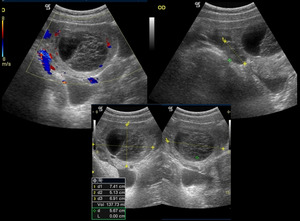
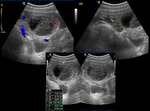
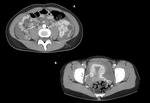
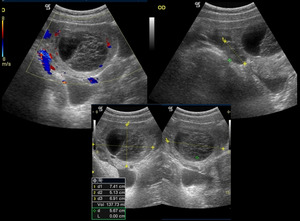
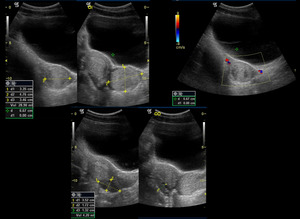
Fig. 3: 12-year-old girl with severe pain in hypogastrium is sent to our service with suspicion of appendicitis. In US demostrated a left ovary increased in size (7.4 x 5.1 x 6.9 cm.), With vascularization present and small follicles peripherals as well as cystic lesion with septa and without flow inside 5.2 x 4 cm, compatible, with hemorrhagic luteal body with a partial torsion of the left ovary.
Small amount of free fluid subhepatic,in Morrison and Douglas spaces and between intestinal loops.
References: Department of Radiology, Hospital Universitario Marqués de Valdecilla - Santander/ES
2.
OVARIAN NEOPLASMS
Ovarian neoplasms commonly have a cystic component and may be benign or malignant.
The solid component is the most statistically significant predictor of malignancy.
Categories are defined by the cell of origin: germ cell tumors,
epithelial tumors,
and stromal tumors.
These neoplasms generally present in postpubertal girls as a result of pain,
increasing abdominal girth,
and symptoms derived from hormonal effects when masses are functional.
2.1.
GERM CELL TUMORS
Benign teratomas comprise 67% of pediatric ovarian neoplasms and are bilateral in up to 25% of cases.
Mature teratomas contain tissue from all three primitive lines: endoderm,
mesoderm,
and ectoderm.
The presence of fat or calcification in the lesion is diagnostic and easily distinguished by CT or MR.
The diagnosis may be slightly more challenging by ultrasound,
but several signs are helpful including the “tip of the iceberg” sign (coarse,
shadowing calcification),
dermoid mesh (linear interfaces representing hair),
and dermoid plug (echogenic nodule with fat,
hair,
and teeth).
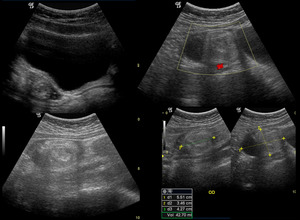
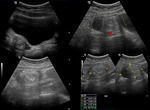
Fig. 4: 10-year-old girl with a hyperechogenic nodule, discrete heterogeneous with well-defined margins on the lateral margin of the right ovary, 2.3 x 2.5 x 1.9 cm, suggestive of teratoma ovarian
References: Department of Radiology, Hospital Universitario Marqués de Valdecilla - Santander/ES
Some teratomas contain immature elements and have potential for recurrence and metastasis.
This subtype may even present in infants and may result in peritoneal spread of disease.
Other categories of germ cell tumors include dysgerminoma,
yolk sac tumor,
choriocarcinoma,
and mixed varieties.
These tumors are indistinguishable by imaging,
but imaging features direct the operative approach and provide preoperative staging.
2.2.
EPITHELIAL TUMORS: cystadenomas and cystadenocarcinomas.
Most tumors in this category are divided into serous and mucinous subtypes,
both of which are often quite large at presentation.
Imaging highlights internal septations,
papillary projections,
and/ or larger solid components.
On ultrasound,
mucinous tumors may have low-level internal echoes from mucoid material.
2.3.
TUMORS OF STROMAL CELL ORIGEN
These tumors include granulosa-thecal cell tumors,
fibromas,
thecomas,
Sertoli-Leydig cell tumors,
and undifferentiated sex cord stromal tumors.
Many are hormonally active and,
therefore,
present earlier than those without function.
Typically,
these tumors are solid,
unilateral,
and contained.
They may appear similar to germ cell tumors without fat or calcium,
but presentation may foreshadow cell origin.
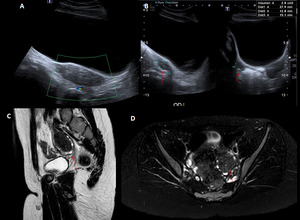
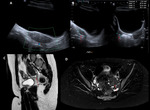
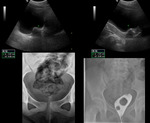
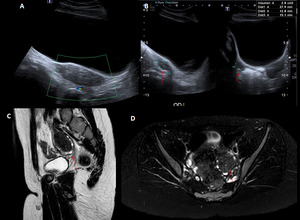
Fig. 5: 9-year-old girl in follow-up for precocious puberty. Fig. A-B. US study:
an increase in the size of the left ovary was observed due to a hyperechogenic mass. Fig. C-D. MR was performed to complete the study, showing a lesion with well-defined borders that caused follicle displacement, with hypointense signal behavior in both pulse sequences, and with a central signal hyperintensity focus. No associated fatty component. Its diameters was 3.8 x 2.1 cm. The lesion had an appearance of fibroma or fibrotecoma. The girl was operated and the result of pathological anatomy was Stromal Sclerosing Tumor.
References: Department of Radiology, Hospital Universitario Marqués de Valdecilla - Santander/ES
2.4.
OTHER RARE OVARIAN NEOPLASMS:
- Aggressive malignancies,
such as small cell carcinoma,
which is usually associated with hypercalcemia.
- Benign entities,
such as hemangiomas.
- Metastatic disease can also involve the ovaries,
either from hematogenous or contiguous spread.
Within this group of malignancies are adenocarcinoma of the colon, Burkitt lymphoma,
alveolar rhabdomyosarcoma,
Wilms tumor,
neuroblastoma,
and retinoblastoma.
3.
OVARIAN CYSTS
The most common adnexal abnormality in the pediatric population is an ovarian cyst.
Ovarian cysts are the most frequent cause of an abdominal mass in the fetus and in the newborn.
An anechoic focus in an ovary is considered a follicle if it is smaller than 3 cm.
A mature dominant follicle may fail to involute appropriately and may enlarge into a functional cyst or corpus luteum.
Follicular ovarian cysts can produce symptoms (mainly pelvic pain of sudden onset) for two reasons: when they rapidly increase in size (above 3cm) or when they become complicated with intracystic hemorrhage,
rupture or ovarian torsion.
An ovarian lesion larger than 5 cm is a risk factor for ovarian torsion.
The echographic appearance depends on the type of complication and the time of evolution:
3.1.
FUNCTIONAL CYSTS
US presents a thin wall and anechogenic content.
Usually,
range from 3 to 8 cm in size.
There should be no colour flow,
nodules or any solid components.
3.2.
HEMORRHAGIC OVARIAN CYST
Severe acute pelvic pain contemporary with the midcycle is clinically suggestive of hemorrhage within a functional ovarian cyst (corpus luteum cyst).
US shows a complex adnexal mass with increased through transmission,
reflecting its cystic nature.
It has different appearances according to the evolutionary phase,
in the early phases is hyperechogenic and in more evolved phases with a declining clot,
multiple septa or liquid-sediment level.
Free fluid can often be observed.
Whether simple or complex,
these lesions are followed by ultrasound to confirm resolution and exclude cystic neoplasm.
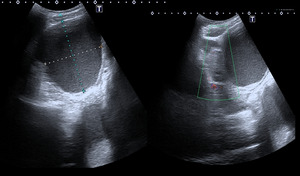
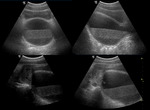
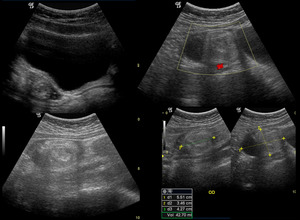
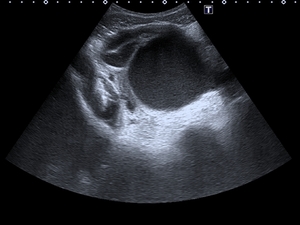
Fig. 6: 12-year-old girl with severe abdominal pain with suspected appendicitis. An ultrasound was performed showing a large right adnexal cystic lesion with echogenic content inside, which was compatible with hemorrhagic cyst.
References: Department of Radiology, Hospital Universitario Marqués de Valdecilla - Santander/ES
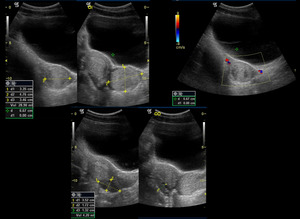
Fig. 7: 15-year-old girl who comes for abdominal pain. It was observed on ultrasound an ovoid lesion dependent on the left ovary, with a volume of 29 cc, and a diameter of 4.7 cm, hyperechoic with small hypoechoic areas inside and avascular. The findings are compatible with hemorrhagic luteum body.
References: Department of Radiology, Hospital Universitario Marqués de Valdecilla - Santander/ES
3.3 RUPTURE OF COMPLICATED CYST: interruption or discontinuity of the cyst wall and increased intra-abdominal free fluid density (direct sign of rupture). The rupture of a functional ovarian cyst can be a diagnosis of exclusion,
since the cyst may collapse completely and not be recognizable in the ultrasound.
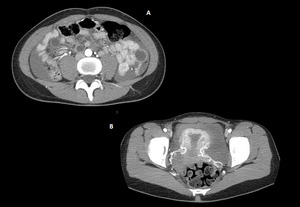
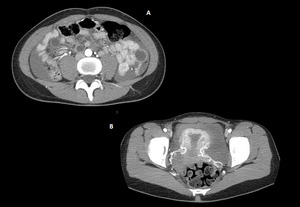
Fig. 8: A 16-year-old girl who presents with right abdominal pain, suspecting appendicitis, was started by performing an ultrasound, afterwards passing to do a scanner given the findings. Extensive hemoperitoneum is observed, with many arterial vessels in the pelvis, with increased density in the vicinity of the uterus, suggesting bleeding of adnexal origin. In this case it was also secondary to a hemorrhagic corpus luteum.
References: Department of Radiology, Hospital Universitario Marqués de Valdecilla - Santander/ES
4.
PELVIC INFLAMMATORY DISEASE
It's very rare for young girls to get pelvic inflammatory disease (PID) before they have their first menstrual period. This is because PID is an infection in the upper reproductive organs,
which really haven't matured before a girl goes through puberty.
Also,
PID generally develops in women who are sexually active,
so children are rarely affected.
Pelvic inflammatory disease in sexually active adolescents is diagnosed based on clinical criteria (acute pelvic pain, cervical motion tenderness,
vaginal discharge,
fever,
and leukocytosis). Ultrasound is useful only to identify complications such as hydrosalpinx or tubo-ovarian abscesses.
Classic imaging findings of tuboovarian abscess and pyosalpinx are complex fluid collections with thick walls and rim enhancement or increased peripheral vascular flow,
often with adjacent inflammatory change and free fluid.
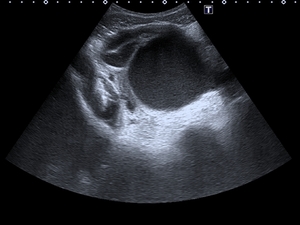
Fig. 9: A 15-year-old girl who came for abdominal pain, found on the ultrasound that depends on the right annex there is a cystic structure with echogenic content inside accompanied by dilation of the tube, which also has echogenic content. The findings are compatible with tubo-ovarian abscess.
References: Department of Radiology, Hospital Universitario Marqués de Valdecilla - Santander/ES
5.
ECTOPIC PREGNANCY
Ectopic pregnancy has the lowest rate among adolescents,
but this age group has the highest reported death rate.
As in adults,
endovaginal US
correlated with quantitative assessment of beta human chorionic gonadotropin is the essential diagnostic test.
6.
VAGINAL FOREIGN BODY
Vaginal foreign bodies are seen in 18% of children with vaginal bleeding and discharge and in 50% of children with vaginal bleeding and no discharge.
A retained vaginal foreign body can be demonstrated at US as a slight indentation of the posterior bladder wall; acoustic shadowing is characteristic but not always present.
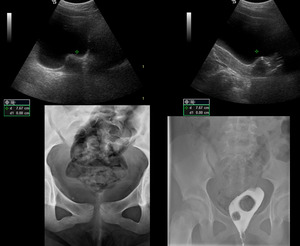
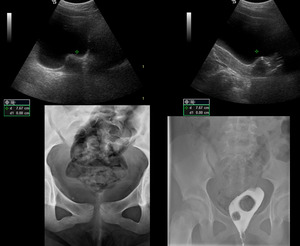
Fig. 10: 10-year-old girl with hypoechoic image with posterior acoustic shadow in vaginal vault, suggestive of foreign body.
It is confirmed the foreign body of 2.5 cm, in the simple x Ray and in the vaginography
References: Department of Radiology, Hospital Universitario Marqués de Valdecilla - Santander/ES
7.
HAEMATOCOLPOS
Haematocolpos is a term given to a blood-filled dilated vagina due to menstrual blood in the setting of an anatomical obstruction,
usually an imperforate hymen. In this condition,
there is no distention of the uterine cavity.
US: Typically shows a fluid distended hypoechogenic mass along the extent of the vagina but not involving the uterus.
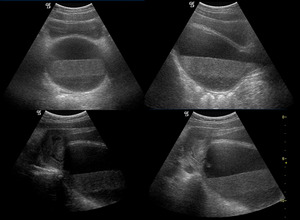
Fig. 11: A 12-year-old girl with a cystic tubular lesion, located between the bladder and the rectum, in communication with the uterine cavity and compatible with hematocolpos.
References: Department of Radiology, Hospital Universitario Marqués de Valdecilla - Santander/ES