Tendinous injuries
a. Lateral epicondylitis
Surgical management of lateral epicondylitis is indicated in patients with persistent debilitating pain after at least 3–6 months of adequate conservative treatment.
Both open and arthroscopic debridement are effective options in the treatment of lateral epicondylitis.
Open procedures
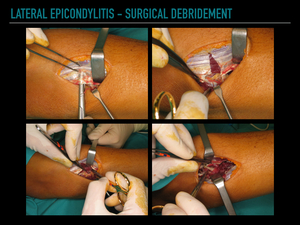
Damaged tendinous tissue displaying macroscopic changes should be debrided.
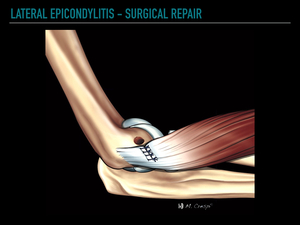
Another surgical option is tendon repair with reinsertion at the lateral epicondyle with suture anchors or bone tunnels,
and microperforations of the epicondyle to promote healing.
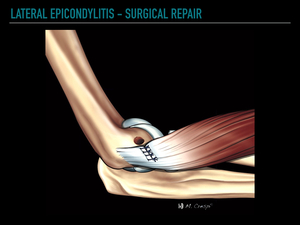
Fig. 1: Drawing illustrating tendon repair technique for the treatment of lateral epicondylitis. Common extensor tendon is reinserted at the lateral epicondyle with suture anchors, and microperforations of the lateral epicondyle are usually performed to promote healing.

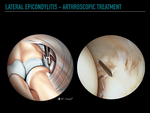
Fig. 2: Arthroscopic release for lateral epicondylitis. Arthroscopic video shows debridement of damaged common extensor tendon, limited to the ECRB, and the adjacent joint capsule.
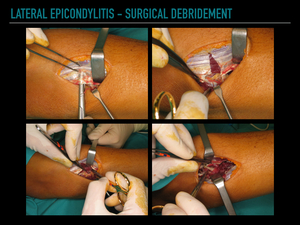
Fig. 3: Open surgical procedure for lateral epicondylitis. The interval between the ECRL and extensor aponeurosis is identified. The underlying pathological ECRB tendon appears dullish gray, the excision should extend till healthy tendon appears.
Percutaneous procedures
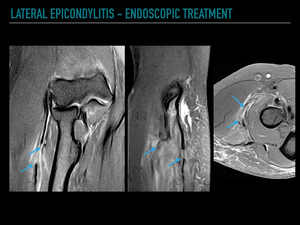
Percutaneous treatment of lateral epicondylitis is address to lengthens the ECRB tendon at the origin of the ECRB or with a Z-plasty at the musculotendinous junction.
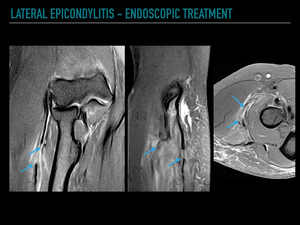
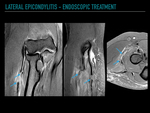
Fig. 4: Endoscopic Z-Plasty procedure for the treatment of lateral epicondylitis. Patient with persistent pain after endoscopic elongation of the extensor tendons at the musculotendinous junction. Coronal PD fat suppressed image shows the surgical defect at the musculotendinous junction (arrows), and focal inflammatory changes.
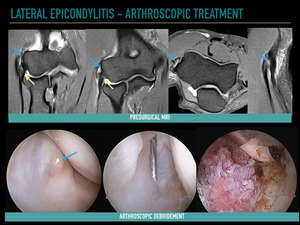
Arthroscopy
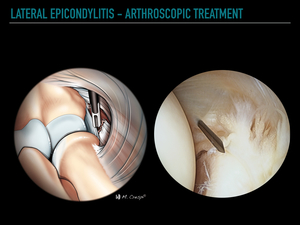
Arthroscopic treatment consists of debridement of the damaged common extensor tendon,
usually limited to the ECRB.
Special care should be taken not to extend the debridement posteriorly to the equator of the radiocapitellar joint to avoid iatrogenic injuries of the lateral ligament complex.
The main advantages of arthroscopic treatment over open techniques are lower morbidity,
early return to prior activity level,
and the evaluation of associated intraarticular injuries.
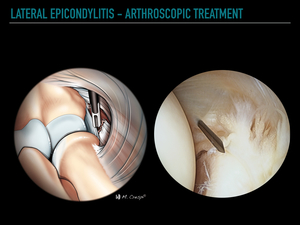
Fig. 5: Arthroscopic treatment of lateral epicondylitis. Drawing and corresponding arthroscopic image illustrating the arthroscopic approach for lateral epicondylitis. Debridement of the damaged tendon is performed through the anterolateral portal.
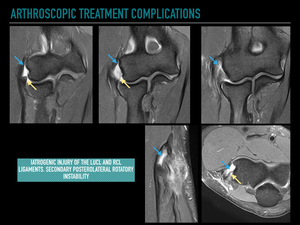
Complications
The main complications of lateral epicondylitis are injuries of the lateral ligament complex with secondary posterolateral rotational instability (PLRI),
and adjacent neural structures (posterior cutaneous nerve).
Other complications common to any surgical elbow procedure,
such as infection,
seromas,
adventitious bursitis,
or adhesive capsulitis,
can occur.
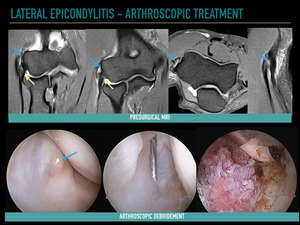
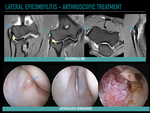
Fig. 6: Arthroscopic treatment of lateral epicondylitis. Preoperative MRI study showing tendinosis and a partial tear of the ECRB (blue arrows). The insertion of the lateral ulnar collateral ligament is preserved (yellow arrows).
Arthroscopic views demonstrating fraying of the capsule overlying the ECRB (arrow), and arthroscopic debridement of the ECRB.
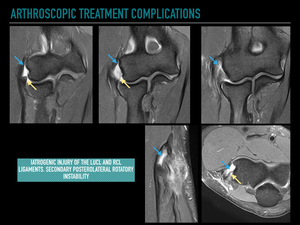
Fig. 7: Postoperative MRI exam shows that the surgery extends too much creating a large tendon defect (blue arrows), iatrogenic injury to the lateral collateral ligament complex (yellow arrows), and secondary posterolateral rotational instability.
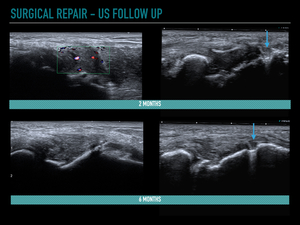
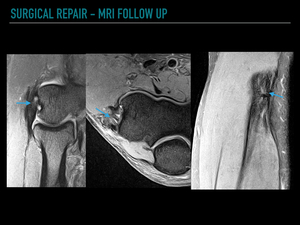
Imaging diagnosis
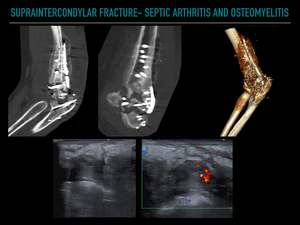
The postoperative imaging assessment of the elbow is usually requested in athletes or manual workers prior to returning to their activity as well as in patients with persistent pain or poor clinical outcomes to rule out complications.
As a general rule,
the assessment of postsurgical patients with imaging methods requires detailed knowledge of the surgical technique performed.
The most useful imaging methods in the postoperative assessment of the elbow are US and MRI.
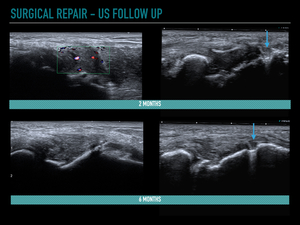
Fig. 8: Normal postoperative ultrasound follow-up in a patient after common extensor tendon repair procedure. Ultrasound study performed two months after surgery showing a diffuse thickening and hypoechogenicity of the repaired tendon, and slight increased tissue vascularity on Doppler. Ultrasound control 6 months after surgery demonstrating that the repaired tendon has more homogeneous fibrillar pattern and increased echogenicity. Note the suture anchor at the lateral epicondyle (arrows).
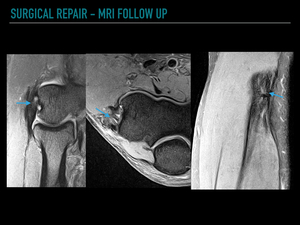
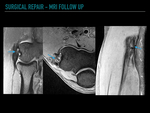
Fig. 9: Normal postoperative MRI appearance of the common tendon after open surgical repair. Coronal, axial and sagittal PD fat suppressed images show a slightly thickened tendon with irregular margins (arrows), and subchondral focal defects at the suture anchor insertion.
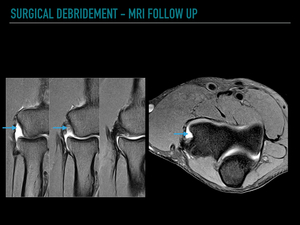
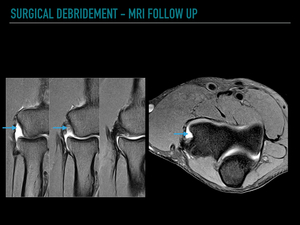
Fig. 10: Normal postoperative MRI appearance of the common tendon tendon after open debridement surgery. Coronal sequential images, and axial images reveal a focal postoperative defect of the ECRB (arrows). This defect should not be misdiagnosed as a retear.
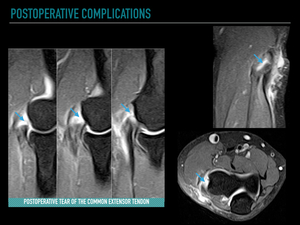
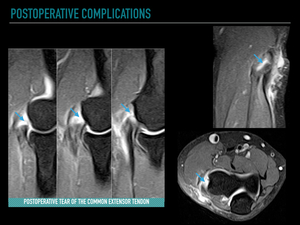
Fig. 11: Postoperative tear of the common extensor tendon. Coronal sequential, axial, and sagittal images show an extensive tear of the common extensor tendon (arrows), and peritendinous soft-tissue edema after an arthroscopic debridement procedure of the ECRB.
b. Medial epicondylitis
Open treatment includes debridement of the tendinosis of the pronator teres and flexor carpi radialis and,
when necessary,
reattachment to the medial epicondyle.
Arthroscopy
Arthroscopic treatment of medial epicondylitis is technically demanding and traditionally thought to be unsafe due to the risk of injuries to the ulnar nerve,
medial antebrachial cutaneous nerve,
or ulnar collateral ligament.
Imaging diagnosis
The normal postoperative and pathological findings,
on both US and MRI,
are essentially the same as those described above for lateral epicondylitis.
Ulnar neuritis is the most common postsurgical complication of medial epicondylitis and is easily detected both in US and MRI.
MRI allows the precise diagnosis of iatrogenic injuries of the anterior band of the medial collateral ligament in the acute phase.
CT and MR arthrography allow a more reliable diagnosis of chronic injuries.
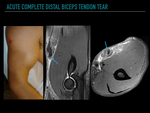
c. Biceps tendon injuries
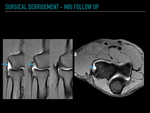
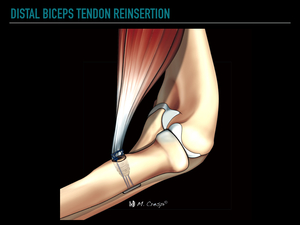
The repair of partial distal biceps tendon (DBT) ruptures consists of debridement of the degenerated tendon and reinforcement of the insertion in the radial tuberosity.
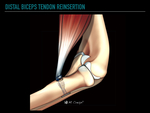
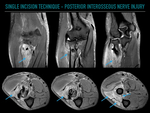
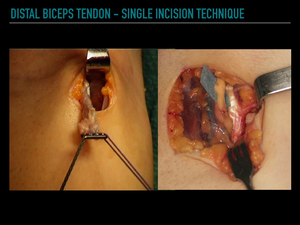
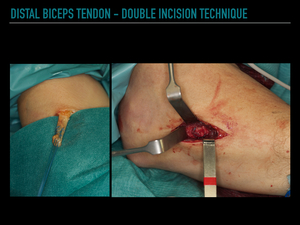
Acute complete ruptures of the DBT can be surgically treated with a single or double incision technique,
with similar functional results.
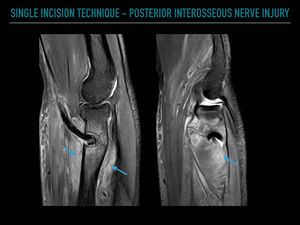
The single incision technique is associated with an increased risk of damage to the lateral antebrachial cutaneous nerve and the posterior interosseous nerve (PIN).
The double incision technique reduces the risk of neurological injury but increases the risk of heterotopic ossification (5-10%).
Re-rupture of the distal biceps tendon repair is uncommon and is usually due to excessive tendon tension,
inadequate fixation,
and poor tendon quality.
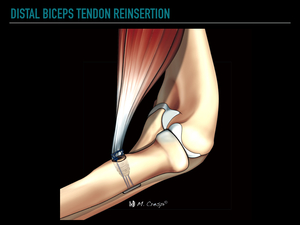
Fig. 12: Drawing illustrating the distal biceps tendon reinsertion technique into the radial tuberosity. The tendon stump is fixed at the radial tuberosity with a variety of techniques, including bone tunnels, suture anchors, interosseous screw fixation, and suspensory cortical button fixation.
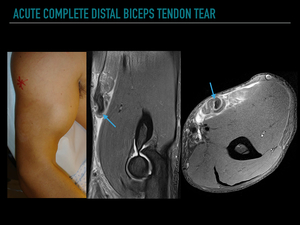
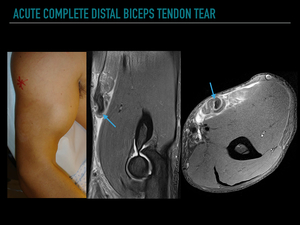
Fig. 13: A 32-year-old-male weightlifter presents with sudden onset of right arm pain. Clinical examination shows a musculotendinous retraction and palpable defect ("Popeye's sign"). Coronal and axial PD fatsat images show a complete tear of the distal biceps tendon and lacertus fibrosus with myotendinous retraction (arrows).
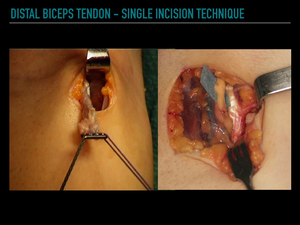
Fig. 14: Acute complete ruptures of the distal biceps tendon can be surgically treated with a single or double incision technique, with similar functional results. The single incision technique is performed by an anterior longitudinal approach, parallel to the ulnar border of the brachioradialis. This technique is associated with an increased risk of damage to the lateral antebrachial cutaneous nerve and the posterior interosseous nerve (PIN); therefore, these should be identified and protected in the surgical procedure to avoid iatrogenic lesions.
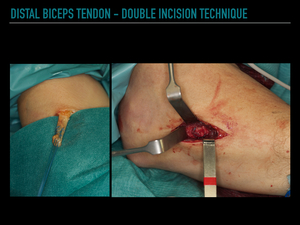
Fig. 15: The double incision technique reduces the risk of neurological injury but increases the risk of heterotopic ossification. A transverse incision is made just distal to the flexion crease of the elbow. The tendon is debrided and surrounded by non-resorbable sutures. A second longitudinal incision is made over the radial tuberosity. The tendon is passed from the anterior to the lateral incision with a tendon passer and then fixed at the radial tuberosity.
Imaging diagnosis
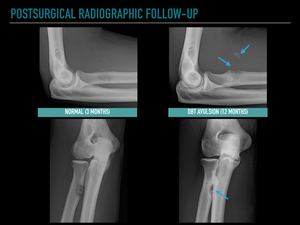
The postoperative imaging assessment of patients with distal biceps tendon surgery should be initiated with conventional radiography.
This may demonstrate postoperative complications,
such as bone avulsions,
widening of the surgical tunnel at the radial tuberosity,
displacement of surgical fixation material,
or heterotopic ossification.
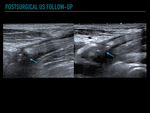
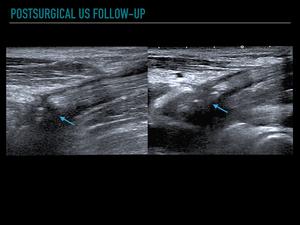
The dynamic capability of the US examination in the evaluation of the distal biceps tendon and neural lesions and the increased detection of heterotopic ossifications makes US the initial method of choice for the postoperative evaluation of the biceps tendon.
On MRI,
a specific FABS position (elbow flexion,
abduction and supination of the forearm) allows a more accurate assessment of the distal biceps tendon insertion.
However,
the combination of the three orthogonal planes usually allows an adequate evaluation of the tendon in most cases without additional projections that may be uncomfortable for the patient.
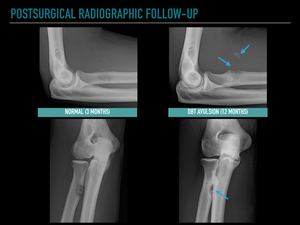
Fig. 16: Postsurgical radiographic follow-up. Antero-posterior and lateral radiographs show normal findings after a distal biceps tendon reinsertion with osseous tunneling, and endobutton fixation at the radial tuberosity. During the radiographic follow up tunnel widening and bone fragment avulsion (arrows) was showed, consistent with complete distal rupture.
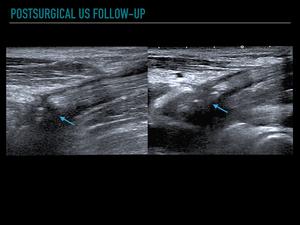
Fig. 17: Ultrasound appearance of a normal distal biceps reinsertion. Longitudinal antecubital and medial approach of the distal biceps tendon show a normal postoperative hypoechogenicity and irregularity at the tendon reinsertion (arrows).
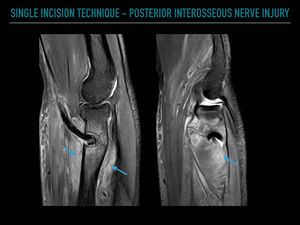
Fig. 18: Patient with distal biceps tendon reinsertion (single incision technique) and postoperative forearm pain and weakness of the extensor muscles. Sagittal sequential MR images show the tendon stump fixed at the radial tuberosity with interference screw and endobutton. Denervation of the extensor muscles of the forearm (diffuse muscle edema) (arrows) secondary to iatrogenic posterior interosseous nerve stretching.
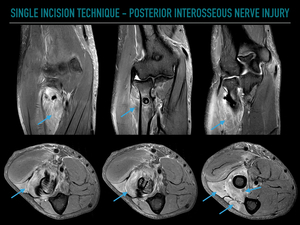
Fig. 19: Coronal and axial sequential MR images of the figure 18 patient showing the extensor muscles denervation (arrows) secondary to iatrogenic posterior interosseous nerve syndrome.
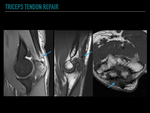
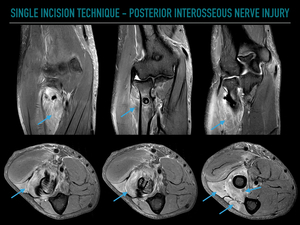
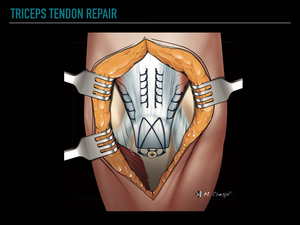
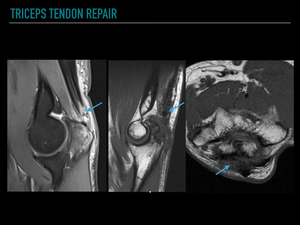
d. Triceps tendon injuries
Partial ruptures greater than 50% and complete ruptures should be surgically repaired,
except in older,
low functioning,
and debilitated patients.
The tendon is fixed distally with transosseous tunnels to obtain anatomical fixation of the tendon.
Chronic ruptures require procedures of tendon reinforcement or augmentation with tendon grafts.
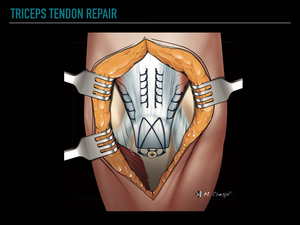
Fig. 20: Drawing illustrating the surgical reinsertion of the complete ruptures of the triceps tendon. Sutures are inserted through the tendon and transosseous tunnels are drilled into the olecranon in order to reinsert the tendon in its anatomical footprint.
Imaging diagnosis
Complications,
such as re-rupture,
flexion contractures,
infection,
and olecranon bursitis from wire suturing,
are rare.
US and MRI both enable detailed evaluation of tendon repair quality and potential complications.
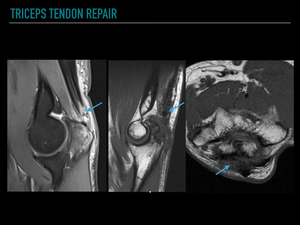
Fig. 21: Normal early postoperative appearance on MRI of anatomical triceps tendon reinsertion. Sagittal PD fat suppressed and axial T1 images show a thickened, and increased signal at the distal tendon (arrows), peritendinous edema, and olecranon bone marrow edema.
2.
Elbow instability
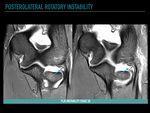
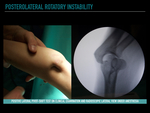
a Posterolateral rotational instability (PLRI)
Lateral collateral ligament complex injuries as a consequence of a single dislocation are generally treated conservatively with good results.
However,
certain patients such as high-level athletes or patients with persistent symptomatic instability following conservative treatment may require surgical treatment.
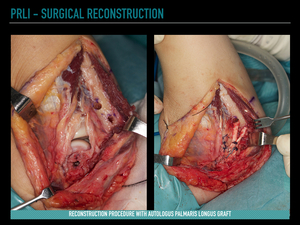
Severe acute injuries and chronic lesions of the LUCL,
without ligamentous tissue of adequate quality to be repaired,
should be treated with open reconstruction with a tendon autograft (palmaris longus,
gracilis,
or triceps fascia) or allograft (semitendinosus).
Traumatic PLRI of the elbow with unstable fractures of the radial head and/or coronoid is an indication for surgery,
and the treatment is primarily aimed at fracture reduction.
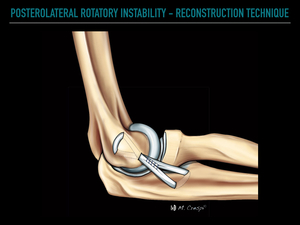
Docking and overlay techniques are the most common techniques used to correct PLRI.
The aim of the graft is to reproduce the posterolateral stabilization of the elbow provided by the LUCL.
The reconstruction must be isometric (tension of the graft maintained throughout the full flexo-extension arc movement),
extracapsular and anatomical,
and it should cover more than 25% of the radial head.
Two holes are created in the supinator crest of the ulna,
separated by at least 1 cm to avoid fractures,
and connected by a transosseous tunnel.
Next,
a hole is opened in the isometric point of the humerus (slightly posterior to the tip of the lateral epicondyle),
from which two divergent "Y" tunnels are drilled.
The graft is passed through the tunnels,
and the ends are fixed with non-resorbable sutures.
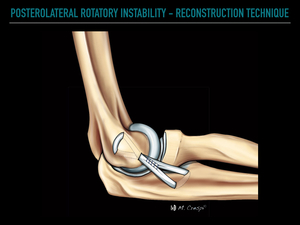
Fig. 22: Drawing illustrating the open reconstruction technique with a tendon graft to correct posterolateral rotatory instability.
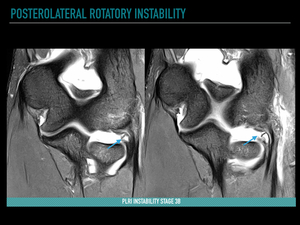
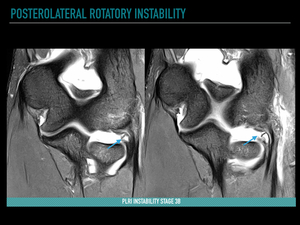
Fig. 23: Posterolateral rotatory instability. Coronal PD fat suppressed images show a complete proximal detachment of the lateral ulnar collateral ligament (arrows).

Fig. 24: Positive lateral pivot-shift test on clinical examination and corresponding radioscopic lateral view under anesthesia. This clinical test is performed with the patient in supine position and affected arm overhead. A valgus force is applied to the supinated elbow, while the elbow is flexed from full extension. For this test to be positive, the elbow should subluxate as it is flexed and subsequently reduce at about 40° of flexion.
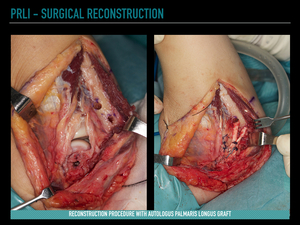
Fig. 25: Surgical images show ligament reconstruction procedure with autologus palmaris longus graft.
Imaging diagnosis
The most frequent graft complications,
such as laxity or tear,
can be identified on US or MRI.
Graft rupture is a rare complication and usually occurs in patients with a new traumatic episode.
In general,
there is no excessive artefact related to the surgical fixation of graft material,
and it is usually necessary to adapt the MRI protocol for artefact reduction.
Given the oblique traject of the graft,
3D FSE isotropic sequences with adapted reconstructions improve direct visualization of the graft and associated complications.
b. Valgus instability
Surgery may be indicated in athletes and manual workers with persistent symptoms of instability and pain despite at least 6 months of adequate conservative treatment.
Primary repair techniques generally yield poor results,
and ligament reconstruction with tendinous grafts are preferred.
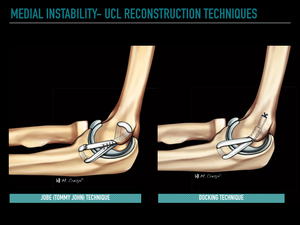
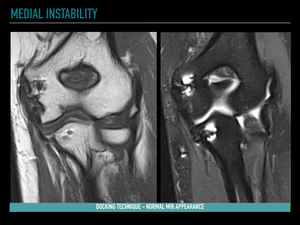
The main reconstructive techniques of the MCL include the modified Jobe technique,
docking technique,
and interferential screw technique.
Jobe described a reconstruction of the MCL (“Tommy John” technique) with bone tunnels in the proximal ulna and medial epicondyle,
with a tendon graft forming a "figure of 8".
This technique involves transposition of the ulnar nerve.
The main complication of this technique is secondary ulnar neuropathy.
Modification of this technique by means of a longitudinal incision of the flexor carpi ulnaris reduces the incidence of this complication,
as neither decompression nor transposition of the nerve is usually performed.
The ulnar tunnel is formed in the sublime tubercle of the ulna,
and the proximal tunnel is formed at the isometric point of the humerus,
immediately anterior and distal to the base of the medial epicondyle.
The "docking" technique is a variant of the modified Jobe technique,
with simplification of the humeral bone tunnels,
which facilitates the graft tensioning.
There is a single proximal tunnel and two small proximal holes for the exit of the sutures.
The hybrid screw technique incorporates the "docking" technique for the humeral fixation with a single bone tunnel and an interferential screw at the ulnar insertion.
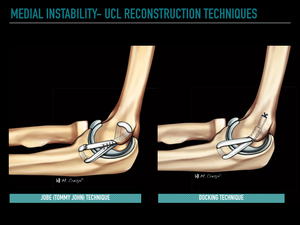
Fig. 26: Drawings showing the Jobe (Tommy John) and docking techniques for ulnar collateral ligament reconstruction.
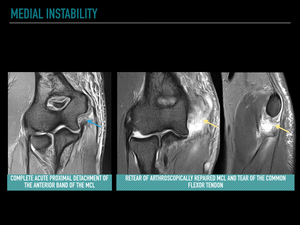
Imaging methods
Conventional radiographs are the primary imaging method used in the immediate postoperative period and in the follow-up period to verify correct anatomical alignment and to detect tunnel or hardware problems.
The imaging techniques of choice for the assessment of ligament reconstruction are US,
MRI and MR arthrography.
US can demonstrate alterations of the tunnels and the possible detachment of hardware fixation of the graft,
as well as partial or complete ruptures.
Dynamic ultrasound evaluation may demonstrate laxity or functional incompetence of the graft.
MRI accurately identifies partial,
complete ruptures,
or anchor detachment.
MRI also allows a precise assessment of the ulnar nerve and potential complications.
MR arthrography is the most useful technique for assessing laxity and partial or complete rupture of the graft.
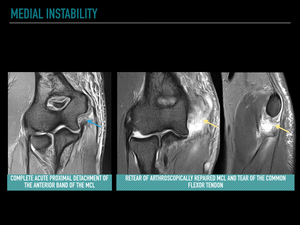
Fig. 27: Acute subluxation in a handball player with history of medial instability treated with arthroscopic repair. Coronal PD fat suppressed presurgical image show a complete proximal detachment of the anterior band of the MCL (blue arrow). Coronal and sagittal PD fat suppressed images after postsurgical traumatism reveal a retear of the repaired MCL and tear of the common flexor tendon (yellow arrows).
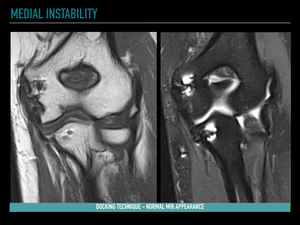
Fig. 28: Normal postoperative MRI findings in a patient with docking reconstruction of the MCL. Coronal T1 and PD fat suppressed images reveal an intact graft with proximal thickening, and artifacts related to suture anchors.
c. Longitudinal forearm instability
An Essex-Lopresti lesion or longitudinal radioulnar dissociation (LRUD) following axial compression injuries of the forearm consists of a combination of radial head fracture,
injury to the interosseous membrane (IOM),
and a lesion of the distal radioulnar joint (DRUJ).
Treatment of acute cases consists of surgical reconstruction of the radial head fracture,
or radial head prosthesis if reconstruction is not feasible.
The treatment of chronic LRUD is extremely complicated and involves a combination of different surgical techniques.
The radial head can be reconstructed with a prosthesis,
the central band of the interosseous membrane with an autograft or allograft (bone-tendon-bone patellar tendon graft) and DRUJ instability with anatomical reconstruction of the distal radioulnar ligaments with tendon grafts.
An ulnar osteotomy to correct the ulnar positive variance is often required.

Fig. 29: Longitudinal instability or Essex-Lopresti injury. Patient with complex fractures of the radial head, interosseous membrane tear, and distal radioulnar ligament injury. The treatment consists on radial head prosthesis and interosseous membrane reconstruction with a bone-tendon-bone patellar tendon graft.
Imaging diagnosis
Postoperative assessment of an Essex-Lopresti lesion is based mainly on conventional X-ray study.
Dynamic radiographic studies during forced grasping may be useful to demonstrate any residual longitudinal instability. In unclear cases,
CT allows assessment of joint reconstruction,
residual deformities,
integration and possible complications of the prosthesis.
CT analysis enables assessment of radial and ulnar tunnelling of the IOM graft and DRUJ instability.
Evaluation of the central IOM and DRUJ grafts should be performed with MRI.
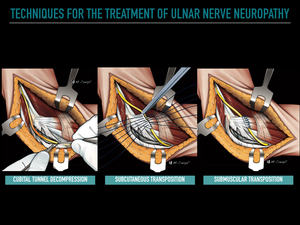
3. Ulnar nerve entrapment
The main surgical procedures include local decompression,
medial epicondylectomy,
and transposition (subcutaneous,
submuscular or intramuscular).
Simple decompression consists of ulnar tunnel retinaculum release and widening of the space between the humeral and ulnar heads of the FCU.
This technique has the primary advantage,
compared with the transposition techniques,
of preservation of neural vascularization.
Decompression of the ulnar nerve can also be performed by medial epicondylectomy.
Transposition techniques involve modification of the path of the nerve from the ulnar tunnel to the anterior aspect of the elbow joint,
and are usually indicated when there is a structural alteration or scar tissue at the ulnar tunnel.
Transposition involves a certain degree of damage to the neural vascularization,
as well as increased susceptibility to pressure damage.
The three types of transposition performed include subcutaneous,
submuscular and intramuscular.
The most commonly performed technique is subcutaneous transposition.
In this technique,
the nerve is transposed to the subcutaneous fat,
into a preformed bed,
and fixed by the fascia lamina.
In submuscular transposition,
the nerve moves below the pronator teres muscle,
which protects it from direct trauma.
Intramuscular transposition is the least commonly used technique,
as it presents more complications and poorer results.
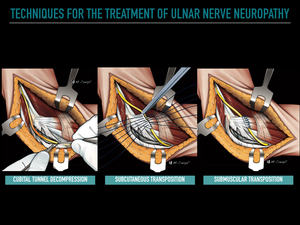
Fig. 30: Drawings illustrating the main techniques for the treatment of ulnar nerve neuropathy. Decompression of the cubital tunnel (commonly associated with epicondylectomy). Subcutaneous transposition. Submuscular transposition.
Complications
Simple decompression and epicondylectomy complications include ulnar nerve instability with friction neuropathy,
and recurrent neuropathy due to postoperative focal fibrosis.
The damage to the neural vascularization in transposition of the ulnar nerve predisposes the patient to transient neuropathy and neural damage by compression.
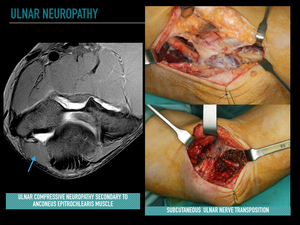
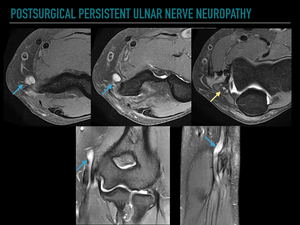
Imaging diagnosis
US and MRI allow assessment of the nerve pathway in the cubital tunnel or subcutaneous,
intramuscular or submuscular rerouting in patients with neural transposition.
The main advantages of US in the assessment of nerve structures are the high spatial resolution,
the possibility of a simple assessment of long segments of the nerve,
and dynamic diagnosis of nerve instability.
The postoperative MRI assessment of the ulnar nerve and the location of the path of the nerve are better analyzed via axial sections.
The size and signal of the ulnar nerve should be evaluated and should not be significantly modified with respect to proximal or distal segments of the ulnar nerve,
and the nerve signal should be similar to the normal median nerve.
The use of 3D neurography sequences allows a more accurate diagnosis of ulnar neuropathy.
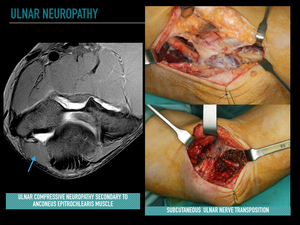
Fig. 31: Ulnar compressive neuropathy secondary to anconeus epitrochlearis muscle.
Axial PD fat suppressed image shows the nerve compression by an anconeus epitrochlearis muscle (arrow). Surgical treatment with resection of the accessory muscle, subcutaneous transposition and fixation with a fascia lamina.
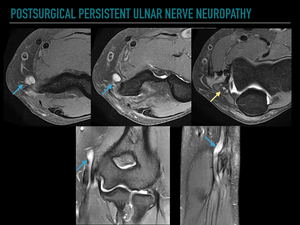
Fig. 32: Persistent ulnar neuropathy after subcutaneous transposition. Consecutive axial PD fat suppressed images from proximal to distal showing the nerve path rerouting. The ulnar nerve is thickened and with increased signal (arrows). Note the compression between the humeral and ulnar heads of the FCU (yellow arrow).
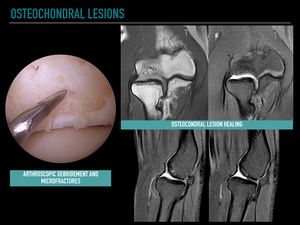
4. Osteochondral Lesions
Surgical treatment is indicated in patients with mechanical symptoms,
unstable fragments,
or intraarticular loose bodies,
as well as after 6 months of conservative treatment failure.
The most common surgical procedures include arthroscopic debridement,
abrasion chondroplasty,
free body removal,
and microfracturing.
In cases of large capitellum defects,
osteochondral transplantation with open surgery should be considered.
Imaging diagnosis
MRI allows assessment of the stability and viability of the fragment,
healing and complications such as subchondral collapse,
osteonecrosis,
free bodies and osteoarthritis.
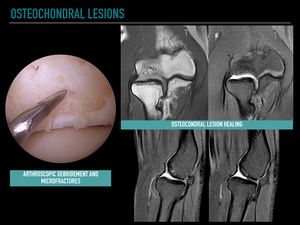
Fig. 33: Osteochondral lesion of the capitellum. Arthroscopic image shows debridement of the osteochondral lesion and microfractures. Postoperative coronal T1 and sagittal PD fat suppressed images confirm osteocondral lesion healing without deformity. Homogeneous layer of fibrocartilage covers the osteochondral lesion.
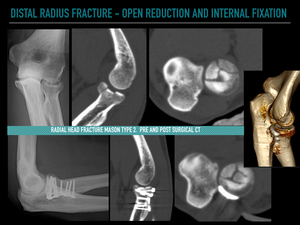
5. Fractures
The complexity of many fractures and fracture-dislocations of the elbow causes a high rate of associated complications.
The complications that are most frequently associated with the failure of surgical treatment and revision surgery include malunion,
non-union,
problems with the materials of osteosynthesis (loosening or displacement),
infection,
osteonecrosis,
neuropathies and instability.
Other complications to be considered in the follow-up of elbow fractures include stiffness,
heterotopic ossification and cutaneous dehiscence.
Imaging diagnosis
The initial postoperative assessment and follow-up of elbow fractures are commonly performed with conventional radiology.
This allows the evaluation of the reduction of the fractures and,
in the follow-up,
evaluation of the displacement or loosening of the osteosynthesis material,
consolidation,
and complications,
such as infection or heterotopic ossification.
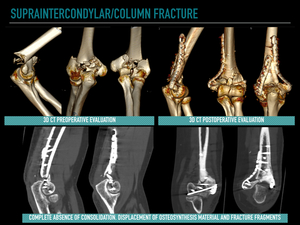
The most important diagnostic technique in the follow-up of fractures and in the diagnosis of possible postoperative complications is CT.
CT allows an accurate assessment of the degree of consolidation,
as well as complications related to the osteosynthesis material,
infection or heterotopic calcifications.
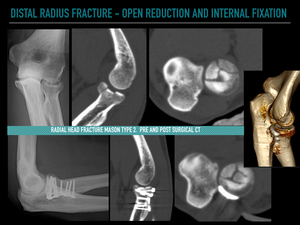
Fig. 34: Radial head fracture Mason type 2. Initial PA plain film shows a comminuted radial head articular fracture, with depressed central fragment. Preoperative sagittal and axial CT images show a four fragment intraarticular fracture with central fragment depression.
Postoperative lateral plain film shows the fracture reduction with a low-profile plate. Postoperative sagittal, axial and 3D CT images show a good fracture reduction, without articular surface deformity.
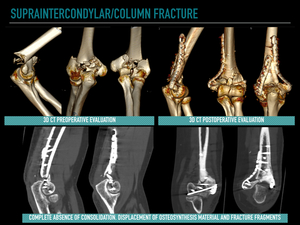
Fig. 35: Preoperative 3D CT images show a complex supraintercondylar column distal humeral fracture. Postoperative CT at six months reveal a complete absence of consolidation, displacement of osteosynthesis material and fracture fragments
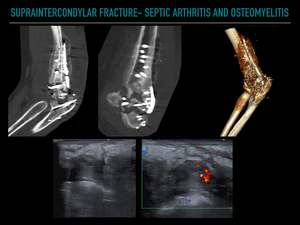
Fig. 36: Complex humeral fracture treated with open reduction and internal fixation using plating technique and osseous graft, complicated with osteomyelitis. Sagittal and coronal CT images show a complete absence of fracture consolidation, periosteal reaction and irregular bone destruction. Doppler ultrasound images show a diffuse septic arthritis of the elbow.
Specific MRI protocols adapted for the reduction of ferromagnetic artifacts allows the evaluation of postoperative complications of fractures.