Upper GI series includes examination of the upper GIT from the oropharynx till the duodenojejunal flexure by single contrast technique,
through administration of barium orally (Diluted light barium) or water soluble low osmolar contrast if there is risk of aspiration; using bottle or though nasogastric tube if the patient unable to drink.
[2]
Once the patient begins drinking,
we obtain an anteroposterior image of the esophagus and then turn the patient to the right lateral position,
We obtain a lateral view of the esophagus and then wait for contrast to pool in the antrum and when the contrast passes through the pylorus and begins to fill the first and second portions of the duodenum,
we obtain a lateral view documenting that the pylorus appears normal and that the duodenum courses posteriorly.
Then the patient is quickly turned supine and an image is obtained as the contrast courses into the duodenum and proximal jejunum with visualization of the Duodeno-jejunal flexure location.
[2]
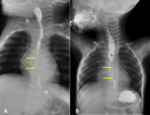
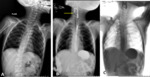
Normal upper gastrointestinal anatomy:
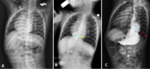
The normal radiological anatomy of the esophagus starting from normal symmetrical appearance of both valleculae and pyriform fossae then the esophagus itself appears as featureless tube filled with contrast,
normal smooth mucosal surface which appears as straight smooth longitudinal folds not more than 3 mm in width along its entire length with three normal indentations found on its anterolateral aspect corresponding to: (1) aortic arch,
(2) left main bronchus,
and (3) left atrium and end at the gastroesophageal junction which should be under the diaphragm.
(Figure 1) [3]
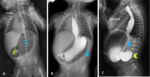
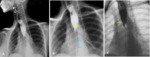
The stomach appears as J-shaped dilation,
divided into 4 parts (fundus,
body,
antrum and pylorus) with smooth Gastric rugae folds that tend to parallel the long axis of the stomach and are about 3 mm in thickness.
The duodenum forms a C-shaped loop around the head of the pancreas,
the first part appears smooth featureless while the rest of the duodenum shows smooth circular mucosal folds till the duodeno-jejunal junction which located to the left side of the first lumbar vertebra.
(Figure 2,
3) [4]
Upper GI series findings in the most common upper GIT pathologies in pediatric:
Congenital anomalies:
Congenital anomalies of the esophagus include esophageal atresia with or without tracheoesophageal fistula which is the most common esophageal malformation [5],
congenital esophageal stenosis,
esophageal duplication cysts and communicating foregut malformations (upper GI series has role in diagnosis and in postoperative assessment (Figure 4)).
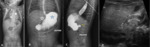
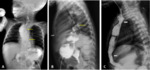
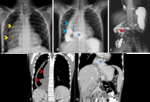
Congenital anomalies of the diaphragm include diaphragmatic hernias (Figure 5),
hiatus hernia (Figure 6,
7,
8).
Congenital anomalies of the stomach include pyloric and antral atresias or stenosis,
Antral mucosal diaphragm,
Microgastria,
Duodenal atresia (Figure 9) or stenosis,
Duplication Cyst and Malrotation (Figure 11,
12,
13),
and infantile hypertrophic pyloric stenosis or gastric outlet obstruction (Figure 10).
In any case with congenital anomaly we must search for other associated anomalies.
Inflammatory disorders:
Esophagitis or gastritis secondary to gastroesophageal reflux disease GERD (Figure 13,
14,
15),
the symptoms of the patients are directly proportionate with the degree of the GERD.
Diffuse inflammatory changes can occur secondary to corrosive ingestion.
Upper GI series can detect complications as post corrosive esophageal stricture.
In addition,
it is essential imaging modality in postoperative follow up (figures 16,
17,
18,
19).
[6]
Moreover,
benign esophageal stricture (figure 20),
are caused by a variety of esophageal disorders,
including eosinophilic esophagitis,
reflux esophagitis (figure7),
Schatzki ring or secondary to post-operative intervention.
[7]
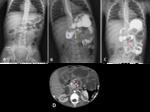
Neoplastic disorders:
Primary gastrointestinal tumors are uncommon in children,
and GI malignancies account for less than 2% of all cases of pediatric cancer.
[8]
Esophageal smooth muscle tumors such as leiomyomas or leiomyosarcomas are rare in children and often multifocal,
leiomyoma in children are usually associated with familial syndromes such as familial leiomyoma or Alport syndrome.
[8].
Alport syndrome is an inherited disease of type IV collagen,
X-linked dominant or less commonly autosomal recessive.
It present in two thirds of patients with diffuse esophageal leiomyomatosis (figure 21).
Diffuse leiomyomatosis is characterized by circumferential hypertrophy of smooth muscle and almost affect the esophagus,
however other gastrointestinal organs can also be affected,
patients often presented with regurgitation,
vomiting and dysphagia.
Constipation with encopresis may be present if the patient has perirectal or perianal hypertrophy,
sensorineural deafness and ocular chnges are a common associated manifestations.
[9]
Gastrointestinal stromal tumors (GIST) are rare mesenchymal tumor which arise from interstitial cell of Cajal and the commonest site to be affected is the stomach (50-70 %),
followed by small intestine (20-30 %),
rectum (10 %) and esophagus (5 %).
[8]
Lymphoma is the most common malignancy affecting small bowel in children and high grade non Hodgkin lymphoma representing 74 % of these tumors.
[8]
Miscellaneous:
Aspiration (figure 22) early recognition and appropriate management of oropharyngeal aspiration (OPA) is important in preventing chronic lung disease.
[10]
Gastric volvulus (figure 5,
6,
13,
23) is uncommon among pediatric and adolescent patients,
volvulus of the stomach is defined as twisting of the stomach over 1800 and can be organoaxial,
mesenteroaxial or combination of the two depending on the axis of rotation.
Can be associated with diaphragmatic eventration,
congenital diaphragmatic hernia,
intestinal malrotation,
wandering spleen,
asplenism and hiatal hernia.
[11]
External esophageal compression (Figure 24) by the nearby surrounding structures.
Iatrogenic esophageal injury: esophageal false passage (figure 25),
“double-lumen esophagus” or “double cardia” is a rare entity,
seldom reported in the literature,
usually as a result of formation of an esophagogastric fistula secondary to reflux esophagitis,
a complicated fundoplication or malignancy.
[12]