Aims and objectives
The addition of digital breast tomosynthesis (DBT) to digital mammography has been shown to improve cancer detection rates [1-4] and lower recall rates [2-7] but prolongs reading time almost two-fold [1,
8,
9],
compared to digital mammography alone.
Therefore,
an artificial intelligence (AI) system (ProFound AI™ ver 2.0; iCAD,
Inc.,
Nashua,
NH/US) based on deep learning was developed to detect malignant soft tissue and calcific lesions in DBT exams.
The algorithm provides outlines of detected lesions in the DBT slices and calibrated lesion-level and case-level...
Methods and materials
A multi-reader,
multi-case (MRMC) study was retrospectively conducted with 24 radiologists and 260 cases with DBT exams. All cases were read by each radiologist both with and without the AI system,
with at least 4 weeks between readings of the same with and without AI.
The 260 cases included 65 biopsy-proven cancer cases with 66 malignant lesions,
65 benign cases with biopsy-proven benign lesions,
21 cases with lesions shown not to warrant biopsy based on additional imaging and 109 BI-RADS 1 or 2 cases without...
Results
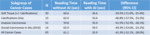
The sensitivity subgroup analysis in Table 1 shows that average radiologist sensitivity improved 6.8% with AI for soft tissue and 6.2% for invasive carcinomas,
with larger improvements of 12.0% for calcifications-only and 14.6% for DCIS.
Of note,
all 95% CIs were above zero,
indicating strength of these improvements.
For all cancer cases,
average radiologist sensitivity improved 8.0% (95% CI: 2.6%,
13.5%) from 77.0% without AI to 85.0% with AI.
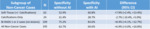
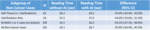
Subgroup analysis of reading time in cancer cases (Table 2) shows that average radiologist reading time...
Conclusion
The purpose of this study was to evaluate the concurrent use of AI with DBT based on mammographic appearance and histopathology.
The results showed larger improvements in sensitivity for calcifications-only lesions and DCIS compared to soft tissue lesions and invasive carcinomas.
Specificity improvements were similar for soft tissue lesions and cases without suspicious lesions,
with no improvement for calcifications-only lesions.
Of interest were the 55.9% reduction in reading time with all non-cancer cases and even 59.1% with BI-RADS 1 or 2 cases that were not...
Personal information
Emily F.
Conant,
MD
Department of Radiology,
Perelman School of Medicine at the University of Pennsylvania,
Philadelphia,
PA/US
[email protected]
Senthil Periaswamy,
Ph.D.
iCAD,
Inc.,
Nashua,
NH/US
[email protected]
Sergei V.
Fotin,
Ph.D.
iCAD,
Inc.,
Nashua,
NH/US
[email protected]
Jonathan Go,
M.A.Sc
iCAD,
Inc.,
Nashua,
NH/US
[email protected]
James Pike,
MSEE
iCAD,
Inc.,
Nashua,
NH/US
[email protected]
Justin E.
Boatsman,
M.D.
Intrinsic Imaging,
LLC,
Bolton,
MA/US
[email protected]
Jeffrey W.
Hoffmeister,
M.D.,
MSEE
iCAD,
Inc.,
Nashua,
NH/US
[email protected]
References
1.
Skaane P,
Bandos AI,
Gullien R,
et al.
Comparison of digital mammography alone and digital mammography plus tomosynthesis in a population-based screening program.
Radiology 2013;267(1):47-56.
doi: 10.1148/radiol.12121373
2.
Friedewald SM,
Rafferty EA,
Rose SL,
et al.
Breast cancer screening using tomosynthesis in combination with digital mammography.
JAMA 2014;311(24):2499-2507.
doi: 10.1001/jama.2014.6095
3.
Sharpe RE,
Venkataraman S,
Phillips J,
et al.
Increased cancer detection rate and variations in the recall rate resulting from implementation of 3D digital breast tomosynthesis into a population-based screening program.
Radiology 2016;278(3):698-706....