The term colitis refers to inflammation of the wall of the colon,
that is represented mainly by an colon wall thickening.
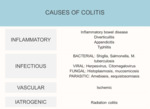
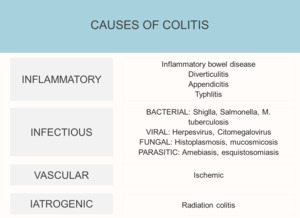
It can be secondary to different causes,
but mostly by infection,
inflammatory bowel disease (Crohn's disease,
ulcerative colitis) or ischemic conditions.
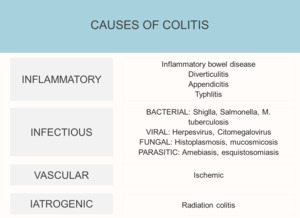
Fig. 1: Causes of colitis
As the computed tomography (CT) has become a major diagnosis tool in the detection and characterization of colonic disease,
imaging techniques play an important role in the diagnosis of colitis.
Normal colon wall
The colon and rectum wall are made up of different layers of tissues that include mucosa,
submucosa,
muscular layer and serosa,
and its thickness values on CT depend on the degree of bowel distension and vary widely in the literature.
In general,
the normal wall thickness should be less than 3 mm.
The colonic wall can vary from 1 to 2 mm when the lumen is well distended,
to 4 mm when the wall is contracted or the lumen is collapsed.
The colon transverse diameter is also variable and it could measure up to 9 cm in the cecum whereas the diameter of the transverse colon is normally less tan 6 cm.
CT findings on colitis
Bowel wall thickening is a common and a non-specific finding in imaging.
CT can be helpful in narrowing the differential diagnosis.
The important features to look for are:
- Length of involvement
- Mural thickening degree
- Enhancement pattern
- Lumen contents
- Mesenteric changes
1.
LENGHT OF INVOLVEMENT.
Each disease has predilection for different parts of the colon,
so we can find right colitis,
left colitis or pancolitis.
2. MURAL THICKENING DEGREE. The diseases that cause the largest bowel wall thickening are Crohn's disease and Pseudomembranous colitis (PMC)
3.
ENCHANCEMENT PATTERN.
There are five categories of attenuation patterns described,
white,
gray,
halo sign,
fat halo sign and black.
White attenuation pattern Fig. 2: The pattern of white attenuation represents rapid contrast material enhancement that uniformly affects the majority of the thickened bowel wall.
Can be caused by two main pathophysiologic events.
The first one is due to vessel vasodilatation in acute inflammatory bowel disease,
and the other one,
is due to the injury to the intramural vessels,
that results in interstitial leakage.
There is an increased permeability and enhancement secondary to the hypoperfusion.
It´s important to distinguish the enhancement from the intramural hematoma that also leads a white pattern image.
Grey attenuation pattern Fig. 2: the thickened bowel shows low homogeneous enhancement and the attenuation is comparable with that of enhanced muscle.
Is the least specific of five attenuation patterns.
Water halo sign Fig. 3: refers to stratification of the thickened bowel wall,
with symmetrically thickened two or three layers.
The "target sign" is a variant of this pattern.
The lower-attenuation layer represents edema and can be assumed to be located in the submucosa,
whereas the inner and the outer rings of the target sign are believed to be the mucosa and the muscular layers.
Water halo sign indicates bowel wall injury,
often of an acute nature,
and rarely manifests malignancy.
Fat halo sign Fig. 3: Stratification with a fat layer (submucosal) in the intestinal wall.
Black attenuation pattern Fig. 4: is equivalent of pneumatosis. Although pneumatosis is usually considered a sign of life-threatening in- jury,
on occasion,
it may not be so.
Any process that is accompanied by a break in the mucosa can introduce intramural gas.
4.
LUMEN CONTENTS.
Fig. 5 Itis important to look for intraluminal blood,
as this finding would support the diagnosis of ischemic colitis.
5.
MESENTERIC CHANGES as enlarged lymphnodes,
edema and engorgement of vessel or fistulas.