Current clinical indications to CMR in DCM can be summarized as follows:
- Accurate assessment of ventricular volumes,
wall thickness and contraction function as well as tissue characterization (pretreatment and follow-up)
- Detection of intracavitary thrombi
- Differential diagnosis between ischemic and non-ischemic DCM
- Differential diagnosis in non-ischemic DCM
- Preimplantation of cardiac resynchronization therapy (CRT)
- Prognostic information (LGE,
T1 mapping,
ECV,
etc.).
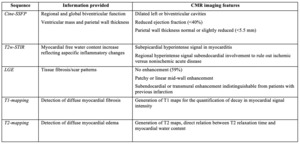
Although the acquisition technique should be tailored to a specific clinical request,
a standard imaging protocol in DCM has to include Cine-SSFP,
T2w-STIR,
T1 mapping,
T2 mapping and LGE.
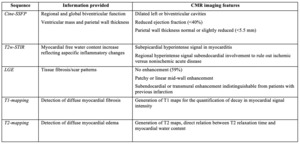
Table 1: Use and significance of different CMR sequences applied for the evaluation of DCM. Modified from Francone[5]
References: Bioimaging and Radiological Sciences, Catholic University, A. Gemelli Hospital - Rome/IT
Ventricular volume and function
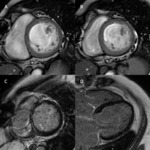
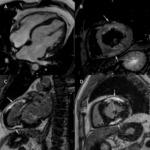
At present CMR can be considered as a reference technique not only for the quantification of ventricular volumes and functional parameters but also for the measurement of the wall thickness.
The primary method used to assess the myocardial function is the steady state free precession (SSFP) technique.
The short-axis images are usually analyzed on a per-slice basis while the Simpson’s method (“stack of disks”) is applied.
One example of the left ventricular contouring is shown in Fig. 1.
Table 2 and Table 3 contain normal values for the left and the right ventricular dimensions and functions according to gender and age (from 20 to 69 years). [9]
The values of EDV of LV higher than 100ml/m2 in men and 95ml/m2in women are considered as values indicating dilatation.
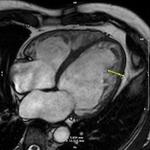
DCM shows globally depressed systolic function but usually no regional wall abnormalities Fig. 2 .
Systolic dysfunction is the most important independent indicator of the outcome in DCM.
The evaluation of diastolic filling allows further identification of subgroups with divergent long-term prognoses.
Previous studies showed that RV mass of DCM patients is comparable to the RV mass of normal subjects,
whereas LV mass value is significantly higher and there is larger trabeculation.
When the disease has progressed though it can also lead to the diffuse myocardial wall thinning of LV (diastolic wall thickness < 5.5 mm).
Edema
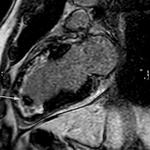
The T2-weighted short-tau inversion recovery (T2w-STIR) imaging with an ECG-gated triple inversion recovery (IR) technique can be used to detect tissue edema when an overlapping active inflammatory process is suspected. Fig. 7
A myocardial inflammation mediated by an acute or chronic viral infection,
direct toxic injury or autoimmune response is one important cause of DCM.
In cases of diffuse edema the T2 mapping technique can help to assess an ongoing myocardial inflammation.
T1mapping & LGE
For the examination of patients,
suspected of having DCM,
late-enhancement sequences have to be performed. Three patterns of DCM-related LGE are reported [10]:
- The most common pattern of LGE (28%–35%) is a linear or patchy midwall LGE representing the intramural layer of septal fibrosis which also histopathologically corresponds to replacement fibrosis and fibrofatty change Fig. 3
- Another possible pattern is a subendocardial and transmural LGE that cannot be distinguished from the typical ischemic pattern
- In major part of patients (59%) there can be no LGE at all,
but this absence can also correspond to diffuse interstitial fibrosis; the absence of LGE does not exclude disease of the heart muscle though
The T1-mapping techniques were recently proposed for the diffuse interstitial fibrosis,
as they allow to identify an increased interstitial accumulation of gadolinium at steady state related to the expansion of the extracellular space with subsequent T1-relaxation time shortening.
The T1 mapping technique also offers the possibility to detect the pre-DCM phenotype. The detection of the pre-DCM phenotype allows an early treatment and delays adverse remodeling. [11]
Tissue fibrosis depicted with T1-mapping techniques positively correlates with the degree of ventricular dilatation and contractility dysfunction.
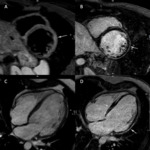
Thrombi
A thrombus is a common complication of DCM that might remain undetected during the transthoracic echocardiography.
The formation of thrombi is triggered by the so-called Virchow’s triad that comes with a hypercoagulability status,
hemodynamic changes (stasis and turbulence) and endothelial injury/dysfunction.
Biventricular stasis facilitates the formation of thrombi in the left ventricle first,
followed by the right ventricle. [5]
CMR is the most preferred diagnostic tool for thrombus detection which looks like a soft-tissue intracavitary lesion.
The signal in the T1 and T2 waited images can vary depending on the age of thrombus:
- Acute: high signal in both T1w and T2w
- Subacute: high signal in T1w and low signal in T2w
- Chronic: low signal in both T1w and T2w
The most sensitive sequence for thrombus detection is the LGE sequence,
here the thrombi appear as black formations because they are avascular and they don’t show contrast enhancement.
It’s possible to use both the conventional (200-300ms according to LL) and the long (>600ms) inversion time (IT). Fig. 4
The organized chronic thrombus may show peripheral enhancement in the LGE images due to fibrous contents.
Differential Diagnosis
The detection of the underlying etiology and an accurate disease monitoring may be crucial for the optimization of individual therapeutic strategies and stratification prognosis.
Ischaemic forms
In LGE images ischemic cardiomyopathy shows areas of subendocardial or transmural enhancement in coronary distribution,
abnormal wall motion might be visible in the affected areas too.
Fig. 5
CMR-perfusion allowed direct visualization of subendocardial ischemia with stress first-pass contrast-enhanced techniques. Fig. 6
Nonischaemic Forms
When it comes to CMR,
a differentiation between various forms of nonischemic DCM is still a complex issue and it’s open for further research.
CMR might offer an additional significant diagnostic contribution as compared to conventional diagnostic tools, above all thanks to its unique tissue characterization capability that narrows down the differential diagnosis. [5,12,13]
In patients with recent-onset DCM,
identification of myocarditis has important clinical implications due to the high potential for LV recovery. Fig. 7
Approximately 5.5%– 9.0% of patients with HCM undergo a burnt-out phase involving the appearance of DCM at MR imaging.
Fig. 8
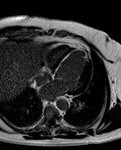
The left ventricular non-compaction cardiomyopathy (LVNC) is a primary CM characterized by deep trabeculations in the LV endocardium. The left ventricular non-compaction cardiomyopathy (LVNC) often presents a phenotype similar to a DCM.
The diastolic non-compacted to compacted ratio (NC/C) of 2.3 has been reported to show high diagnostic accuracy for distinguishing pathological LVNC from various degrees of non-compaction observed in healthy,
dilated and hypertrophied hearts.
Fig. 9

![Table 1: Use and significance of different CMR sequences applied for the evaluation of DCM. Modified from Francone[5] References: Bioimaging and Radiological Sciences, Catholic University, A. Gemelli Hospital - Rome/IT](https://epos.myesr.org/posterimage/esr/ecr2019/148895/media/798106?maxheight=150&maxwidth=150)

![Table 2: Left ventricular parameters, by age and gender [mean ± SD (lower, upper limits*)]. Modified from Kawel-Boehm N et al.
* = calculated as mean ±2*SD References: Bioimaging and Radiological Sciences, Catholic University, A. Gemelli Hospital - Rome/IT](https://epos.myesr.org/posterimage/esr/ecr2019/148895/media/798073?maxheight=150&maxwidth=150)
![Table 3: Right ventricular parameters, by age and gender [mean ± SD (lower/upper limits*)] Modified from Kawel-Boehm N et al.
* = calculated as mean ± 2*SD. Modified from References: Bioimaging and Radiological Sciences, Catholic University, A. Gemelli Hospital - Rome/IT](https://epos.myesr.org/posterimage/esr/ecr2019/148895/media/798072?maxheight=150&maxwidth=150)