Type:
Educational Exhibit
Keywords:
Observational, Not applicable, Infection, Connective tissue disorders, Atelectasis, Structured reporting, Observer performance, Comparative studies, Image manipulation / Reconstruction, CT-High Resolution, CT, Thorax, Respiratory system, Lung, Chest
Authors:
U. S. Umer, S. Alam, S. Gul, S. Ghulam ghaus, A. Nawaz Khan, H. Abid, S. Iqbal, K. Nawab; Peshawar/PK
DOI:
10.26044/ecr2020/C-05643
Background
Introduction to Small airways and Bronchiolitis:
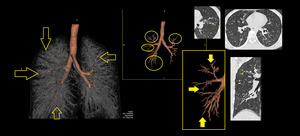
Small airways are bronchioles that do not contain cartilage and have an internal diameter of 1. These small airways are located between the fourth and the 14th generation of the tracheobronchial tree, are only visualized on CT images when diseased ( Fig. 1 ) and comprise the smallest air conducting membranous bronchioles and respiratory bronchioles, which open into the gas-exchange apparatus (the alveoli)2.
Bronchiolitis or small airway disease is a generic term used clinically to describe various inflammatory diseases of the bronchioles. Small airways have been called the silent zone 3. Small airways appear particularly vulnerable because many particles and infectious agents may be deposited there and because of their narrow lumen make them more susceptible to complete obstruction as compared to proximal larger airways. These diseased airways are visible on HRCT as dilated, air-filled, branching, tubular or ring-like structures in the lung periphery by wall thickening and dilation. Abnormalities that involve bronchioles may originate from the bronchioles or may result from extension of disease that involve mainly the larger bronchi such as chronic bronchitis and bronchiectasis or the lung parenchyma, such as bronchopneumonia or organizing pneumonia 4.
MDCT in diagnosing small airway diseases:
Multidetector computed tomography (MDCT) is a powerful diagnostic tool in the assessment of both large and small airway disease 5. High Resolution Computed Tomography (HRCT) is the imaging technique of choice for suspected bronchiolitis ( Fig. 1 )
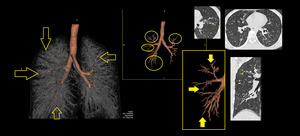
Fig. 1: 3D Volume rendered CT Bronchogram images and reformatted cross sectional volume images labelled with circles and arrows showing the location and abnormality of peripherally located small airways. There is bronchiolectasis, bronchiolar wall thickening giving appearance of serrated margin on bronchogram images and patchy mosaic attenuation alongwith small centrilobular nodules seen on cross sectional images.
Role of HRCT in recognizing specific signs of disease process:
The spatial resolution on a HRCT scan is ∼0.6–1 mm, which allows direct assessment of medium-sized airways (diameter 2–2.5 mm), but not of smaller airways. There are certain signs of diseased small airways, with which they can be identified on images. Small airway disease (SAWD) may show direct or indirect signs on a CT scan. Representative CT scan images are presented in Fig. 19 .