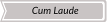
WB-MR acquisition protocol
WB-MR are performed on a 1,5T scanner. Patient is positioned supine headfirst, afterwards a 20-channel head-neck coil, two 18-channel body coils (covering the thoracic and abdominal-pelvic district and the femurs) are connected in combination with a 24-channel spine coil mounted directly on the bed scan.
Scan lasts approximately 45min.
No contrast agent is administered.
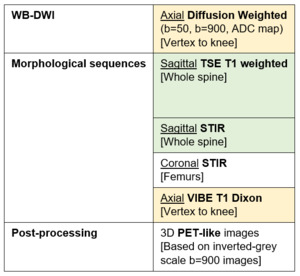
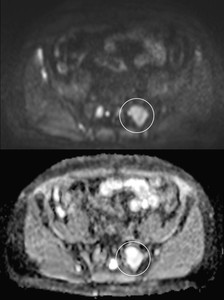
Fig. 1: WB-MR acquisition protocol
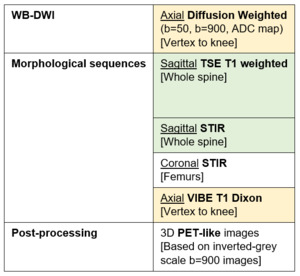
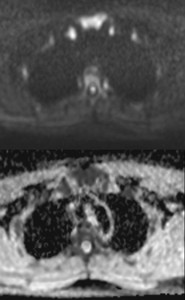
Fig. 2: Axial DW, top to bottom: b=50, b=900, ADC map
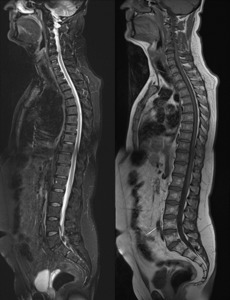
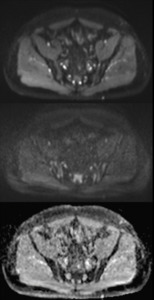
Fig. 3: Morphological sequencences, left to right sagittal STIR and TSE-T1w

Fig. 4: Morphological sequences, coronal STIR
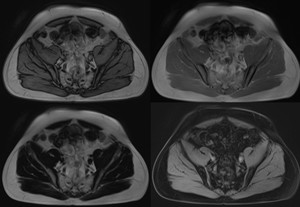
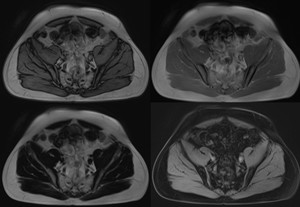
Fig. 5: Morphological sequences, axial VIBE T1 Dixon. Left to right, top to bottom: out-of-phase, in-phase, fat only, water only
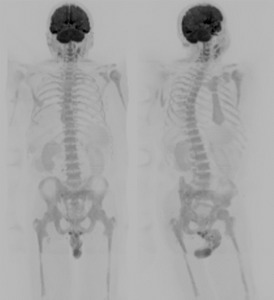
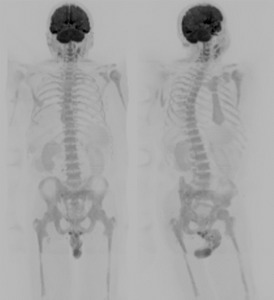
Fig. 6: Post-processing, 3D PET-like images
LD-CT acquisition protocol
LD-CT are performed on a 320-detector row scanner, scan extends from vertex to proximal tibia.
Scan time is approximately 45s; cumulative dose is about 4,5mSv.
No contrast agent is administered.
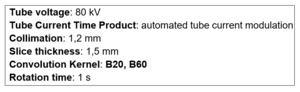
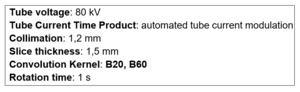
Fig. 7: LD-CT acquisition parameters
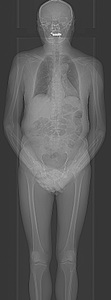
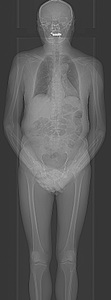
Fig. 8: LD-CT topogram
WB-MR findings
Bone marrow signal intensity is variable and depends on the preponderance of one of its components (haematopoietic marrow, marrow adipose tissue and supportive stromal cells).
Compared to the other radiologic techniques, MR can better detect early anomalies or infiltration of marrow thanks to elevated contrast resolution.
DW-MR, moreover, allows to evaluate cellular density and viability, for these reasons WB-MR including DWI is considered the most sensitive technique for marrow involvement detection.
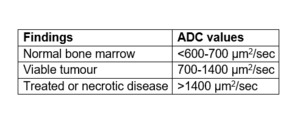
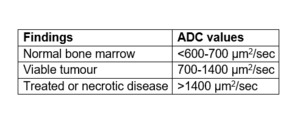
Fig. 9: Approximative ADC values related to bone marrow findings
The evaluation of DW images is based on comparison between b=900 images and corresponding ADC map.
MM shows different pattern of presentation:
- Focal: focal lesions, greater of 5 mm, hyperintense (compared to adjacent muscles) on b=900 images and slightly hyperintense compared to background marrow in ADC.
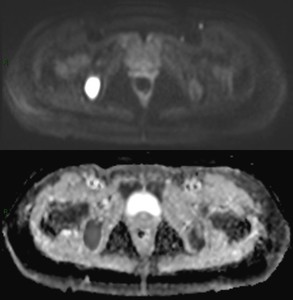
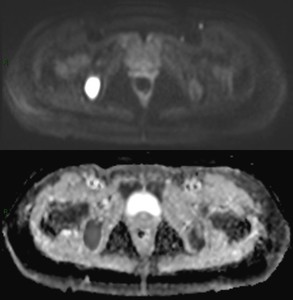
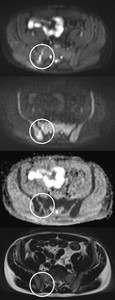
Fig. 10: Focal lesion in right ischial bone
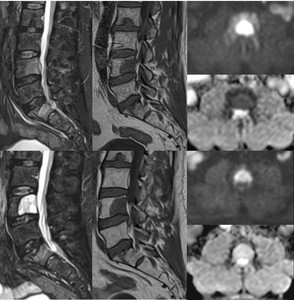
- Diffuse: diffusely higher signal intensity of bone marrow in b=900 with ADC that is similar to soft tissues.
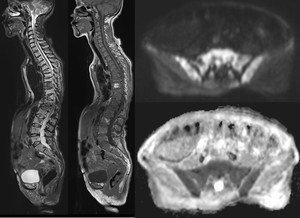
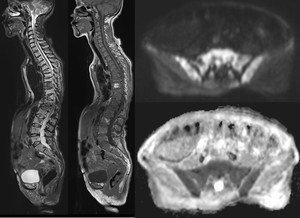
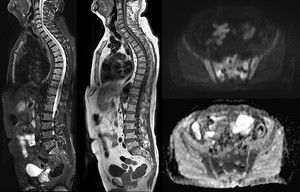
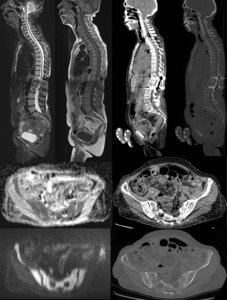
Fig. 11: Diffuse pattern of infiltration in all the segments of the spine
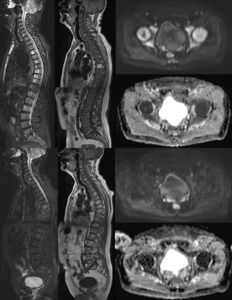
- Focal on diffuse: focal hyperintense lesions in b=900 images and hypointense in ADC map in a hypercellular-background marrow.
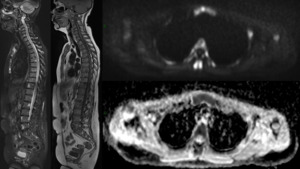
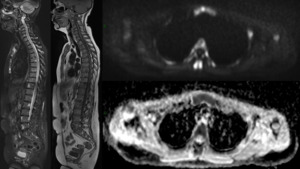
Fig. 12: Multiple focal lesions in diffusely infiltrated vertebral bodies
- Micronodular: tiny nodular areas of pathological bone marrow infiltration with preserved normal marrow between them.
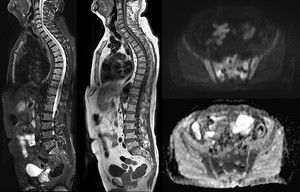
Fig. 13: Micronodular pattern of infiltration
High MR contrast resolution allows also to show paramedullary (presence of pathological tissue in continuity with marrow disease) and extramedullary (pathological tissue not in continuity with disease) extension of disease without mean of contrast administration.
MRI is the preferred modality to evaluate suspected pathological fractures as it demonstrates superior contrast resolution and subsequently better detection of bone marrow involvement.
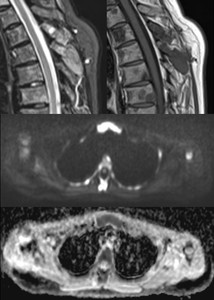
Fig. 14: Paramedullary disease in a dorsal spinous process
Pathological fractures usually demonstrate expansion of the fractured vertebral body, epidural and/or paraspinal soft tissue mass and discrete lesions within the bone; signal intensity is inhomogeneous because of the geographic replacement of normal marrow.
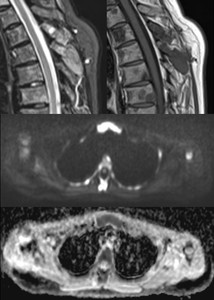
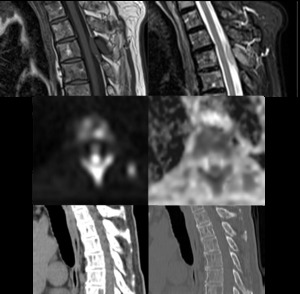
On DW-MR, pathological fractures usually show impaired diffusion. When conventional MRI is combined with DW-MR the diagnostic accuracy and specificity in the evaluation of suspected pathologic fractures improves.
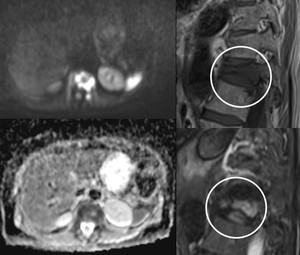
Fig. 15: Pathological fracture of D12 showing impaired water diffusion in the left half vertebral body
CT findings
CT mainly highlights alterations of bone mineralization such as cortical or trabecular disease, rather than marrow infiltration.
On LD-CT traditional MM lesions appear as osteolytic, sharply defined (punched-out) areas with no sclerotic rim.

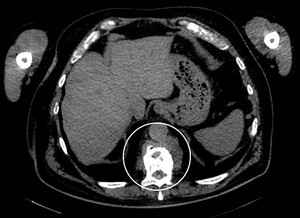
Fig. 16: Multiple lytics lesions on both iliac bones and sacrum
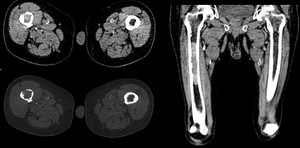
Another kind of lesions detectable on LD-CT are hyperattenuating lesions, i.e. hyperdense tumour deposits in medullary cavities of peripheral skeleton that appear as well circumscribed focal areas of higher density compared to other areas of trabecular bone; they usually show endosteal scalloping of the cortex.
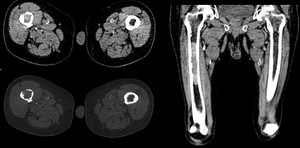
Fig. 17: Hyperattenuating lesion on right femoral diaphysis
LD-CT has a limited role in the detection of diffuse marrow infiltration: it is difficult to differentiate it from osteopenia (especially if marrow infiltration grade is low) as they both appear as bone demineralization.
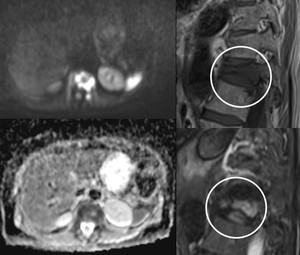
This technique is able to reveal para/extramedullary disease and is typically used to guide biopsy of soft-tissue lesions.
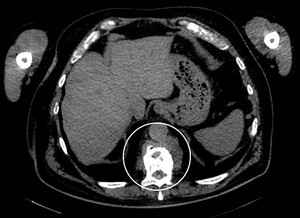
Fig. 18: Paramedullary lesion of D11
In the evaluation of pathological fractures CT provides excellent information about the fracture margins and architectural integrity of the bone.
In a pathological fracture bone is characterized by destructive alteration of the cortex; on the contrary a benign fracture shows fracture lines with sharp borders and retropulsed fragments.
Comparison between WB-MR and LD-CT
WB-MR findings only
WB-MR, thanks to DW sequences, is the only radiologic technique able to differentiate active disease from treated/necrotic disease. Active disease (focal or diffuse) shows high signal on b=900 images and low signal in ADC map, on the contrary, treated/necrotic disease shows high signal in both b=900 images and on ADC map.
This unique characteristic allows to precociously assess response to therapy (after 3 months) in order to evaluate whether therapy is effective or not, and relapse, even in treated lesions.
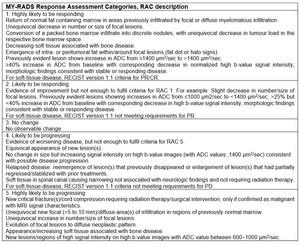
MY-RADS guidelines recommends assigning a Response Assessment Category (RAC) according to anatomic regions. RAC should use a five-point scale:
- Highly likely to be responding
- Likely to be responding
- No change
- Likely to be progressing
- High likely to be progressing
Each category is further described in MY-RADS Table 3, reported in Fig.19
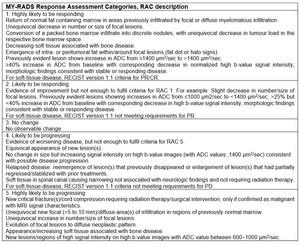
Fig. 19: MY-RADS Response Assessment Categories, reported from MY-RADS Tabele 3
since MM lesions rarely show sclerotic rim as sign of healing, therefore, after treatment it is not possible to establish if disease responded to therapy. LD-CT is able to identify progression of disease only if a new unequivocal lesion appears.
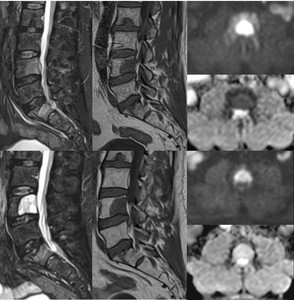
Fig. 20: Focal lesion in L4 at baseline and 4 months after chemotherapy
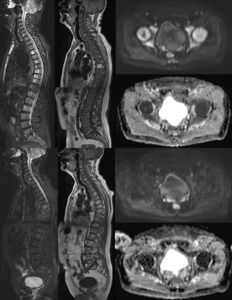
Fig. 21: Focal on diffuse pattern at baseline; after chemotherapy no impaired diffusion and reappearance of yellow marrow
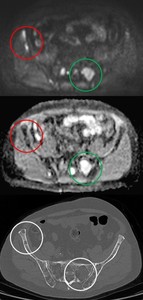
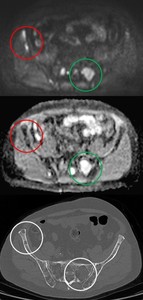
Fig. 22: Response assessment: DW-images shows pathological lesions (encircled in red), and healed lesion (encircled in green); CT does not allow evaluation of lesion vitality
As previously said, WB-MR with DWI is the only radiological technique able to show bone marrow infiltration and viability.
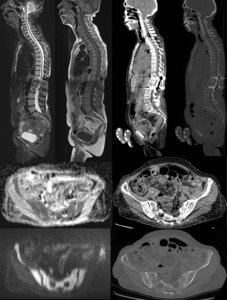
Fig. 23: DWI demonstrates diffuse increased pathological cellularity; CT only shows demineralization
WB-MR findings better than LD-CT
Both WB-MR and LD-CT are able to identify para/extra-medullary extension. However, WB-MR contrast resolution is significantly higher compared to LD-CT (especially when no contrast is administered) and provides a better depiction of spinal roots and spinal cord highlighting spinal cord involvement.
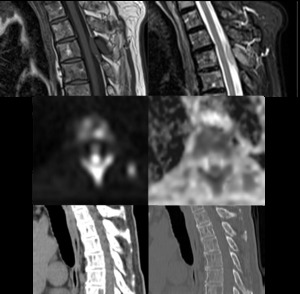
Fig. 24: Paramedullary lesion with intracanalar extension easily recognisable in MR, not evaluable with CT
LD-CT findings better than WB-MRI
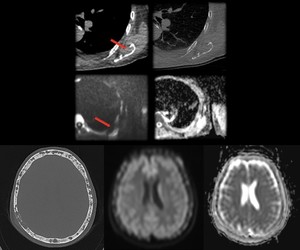
CT scan has a superior spatial resolution than WB-MRI; this allows a better detection of small focal lesions in flat bones (e.g. skull, scapulae). Moreover, in our experience, this technique proved to be superior in the evaluation of the ribs. In WB-MRI, images of thoracic district are acquired in free breathing and this leads to motion artefacts; in LD-CT, instead, images are acquired during inspiratory apnoea resulting in less artefacts and sharper margins.
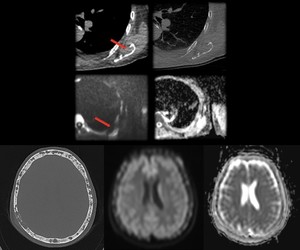
Fig. 25: Top row: lesion on left scapula with cortical and cancellous bone involvement.
Bottom row: multiple focal lesions on skull bones.
WB-MR pitfalls
- T2 shine-through effect: high signal in high b-value images due not to impaired water diffusion but to high T2-native signal.
- Breath artefacts: DW-images are acquired in free breathing causing motion artefacts, reducing quality of images in thoracic district.
- Coil proximity artefacts: high signal on body regions extremely close to coil may represent a false positive.
- Diffuse marrow reconversion due to G-CSF: mimicker of diffuse marrow infiltration; it is important collect anamnestic data to contextualize findings.
- Trephine tract: altered signal on posterior iliac crest may be the result of bone marrow biopsy.
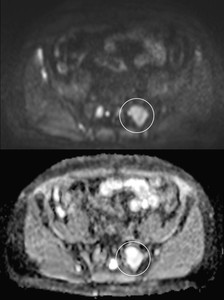
Fig. 26: Lesion treated with radiotherapy. High signal in b=900 without impaired diffusion due to necrosis
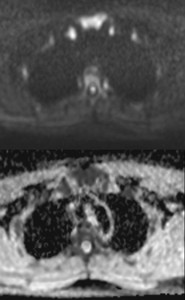
Fig. 27: High signal in sternum and clavicles close to coil resulting in false positive
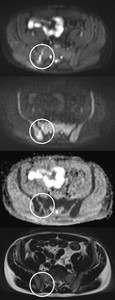
Fig. 28: Trephine tract is recognisable in right posterior iliac crest