Relevant anatomy:
External Auditory canal.
Extends from the auricle to the tympanic membrane, the lateral portion fibrocartilaginous and the medial portion bony.
The tympanic membrane normally should only be faintly discernible on CT. A perforation appears as a focal defect.
Mastoid.
The mastoid air cells are divided by bony septations.
In the central superior aspect is a larger cavity devoid of septations, termed the mastoid antrum. The mastoid antrum communicates with the epitympanum via the aditus ad antrum.
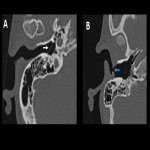
Middle ear.
A cavity within the petrous portion of the temporal bone.
The middle ear can be subdivided into:
- Epitympanum (superior to the level of the tympanic membrane).
- Mesotympanum (at the level of the tympanic membrane).
- Hypotympanum (inferior to the level of the tympanic membrane).
Its lateral border of the middle ear is formed by the scutum and tympanic membrane. The lateral portion of the epitympanum located between the scutum and the ossicles and inferior to the lateral malleal ligament is termed Prussak space.
Its superior border is formed by the tegmen tympani, a thin bony plate that separates the middle ear from the middle cranial fossa. More inferiorly is the opening to the eustachian tube.
Its medial border is formed by the otic capsule, the dense bone encasing the labyrinthine structures of the inner ear, with the inferior portion over the cochlea termed the cochlear promontory.
The oval window, where the stapes attach, is roughly superior to the cochlear promontory.
Superior to the oval window is the tympanic segment of the facial nerve, coursing from anterior to posterior.
The round window serves as a boundary between the basal turn of the cochlea anteriorly and the round window niche posteriorly. The round window niche may obscure complete direct visualization of the round window membrane during routine cochlear implantation.
The posterior margin consists of two outwardly directed recesses separated by a bony protrusion called the pyramidal eminence; the recess lateral to it is the facial nerve recess, and the recess medial to it is the sinus tympani.
The ossicular chain is located almost entirely in the mesotympanum. Consisting of:
- The malleus (Head, neck, anterior process, lateral process, and manubrium).
- Incus (Body, short process, long process, and lenticular process).
- Stapes (Head, anterior crus, posterior crus, and footplate).
Inner Ear.
Consist of the osseous labyrinth encased within the dense otic capsule.
The structures of the osseous labyrinth include the cochlea, vestibule, and the three semicircular canals (superior, posterior, and lateral).
The cochlea is spiral-shaped, comprising a wide basal turn, middle turn, and a small apical turn, for 2.5-2.75 turns. They are separated by bony interscalar septae. In the center is the modiolus, a conical structure of spongy bone containing the spiral ganglion.
Internal Auditory Canal (IAC).
The facial nerve courses along with the anterosuperior compartment of the IAC, the passes into the facial nerve canal in the temporal bone.
The cochlear nerve courses along with the anteroinferior compartment of the IAC, then through the cochlear fossette into de modiolus.
The superior and inferior vestibular nerves course through the posterior half of the IAC.
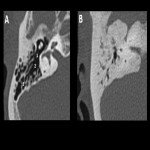
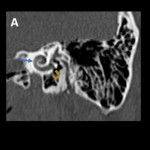
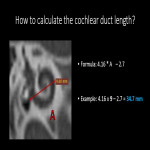
Evaluation of cochlear duct length.
It can be used in preoperative settings to select the properly sized electrode for the patient. This selection of electrodes is crucial as the electrode must provide proper cochlear coverage.
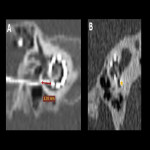
Alexiades et al proposed a formula using computed tomography measurement of basal turn diameter:
Formula: 4.16(A) – 2.7
Where A: Corresponds to the measurement from the center of the round window to the far most extension of the basal turn.
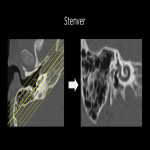
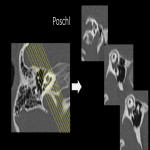
High-Resolution Computed Tomography Protocol:
CT of the temporal bone must be performed at a high-resolution and small field of view.
Thin imaging slices (0.5 mm), to be able to visualize the small, fine structures of the temporal bone to maximal detail.
Understanding the surgical approach:
Standard surgical technique:
- Retroauricular incision.
- Creation of a periosteal pouch in occipital direction to insert the receiving part of the implant.
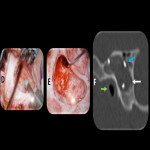
- Partial mastoidectomy with exposure of the posterior wall of the auditory canal, the mastoid course of the facial nerve, and the canal of the chorda tympani.
- Creation of a bone bed to insert the implant at 1 cm behind and above the sinus dura angle.
- Creation of a tunnel to the mastoid in projection on the sinus-dura angle to securely insert and fix the electrode.
- Performance of the posterior tympanostomy by removal of the bone between the bone-covered facial nerve and the chorda tympani.
- Insertion of the implant and positioning of the electrodes.
- Preparation of the round window membrane with the removal of the bone, if needed, to completely visualize the membrane.
- Opening of the cochlear by incisions of the round window membrane or cochleostomy.
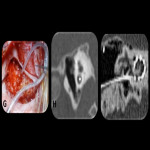
- Insertion of the electrode carrier. Generally, this should be performed in an atraumatic and slow procedure. The selected insertion depths depend on the cochlea's size and the dimension of residual hearing.
- To avoid perilymph fistula, secure closure of the cochlea is essential. Muscle pieces can be placed around the electrode opening.
- Positioning of the electrode carrier.
- Intraoperative electrophysiology is obligatory for the intraoperative functional control of the implant.
- Appropriate wound closure in several layers to securely cover the implant.
- Intraoperative control of the electrode position by radiography to identify insertion failures in time and to correct them in the same session.
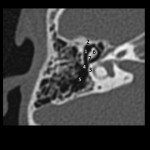
Postoperative imaging:
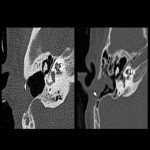
Is required when a malfunction of the device is suspected and to confirm the correct position of the implanted electrode.
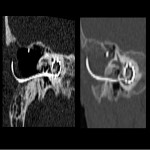
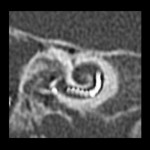
For optimal evaluation of the electrode, a paraxial mid-modiolar plane is selected using multiplanar reconstructions.
The electrode array is intended to be placed in the scala tympani with close contact with the organ of Corti.
Depending on the type of implant and length of the cochlea, the location of the first electrode contact may be located 3-4 mm from the round window opening.
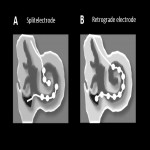
Are two electrodes that are independently implanted in the basal and in the middle turn. (Used in patients with a cochlea ossification/fibrosis and far-advanced otosclerosis).
Insertion through a cochleostomy near the apex.
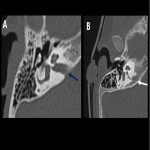
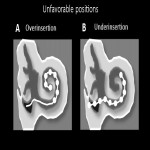
Unfavorable positions:
- Over insertion: This can be recognized when the most proximal contact of the electrode is located more than 3-4 mm from the round window/cochleostomy.
- Under insertion: Exposes several contacts of the electrode array outside of the cochlea. May result in a functional impairment because the external electrode contacts will not be able to stimulate the spiral ganglion cells.
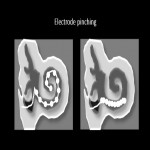
- Electrode pinching: When the electrode array is inserted with too much force or cannot pass further into the cochlea duct a severe accordion-like pinching of the electrode array may be observed.
- Tip fold-over: Electrode tip fold over in the cochlea may lead to the rupture of the basilar membrane.