To carry out a differential diagnosis (DDX) with a practical approach, we will include adrenal lesions into four groups according to their radiological appearance: small adrenal masses, large solid masses, and cystic lesions.
The general characteristics of adrenal pathology and the histology are explained in the body of the text. Most of the radiological findings are explained in the images through examples.
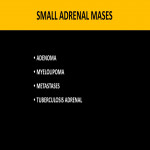
1. SMALL MASSES
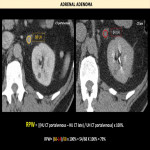
1.1) ADENOMA:
It is the most frequent adrenal tumor, representing a common finding in CT and magnetic resonance imagin-MRI-. Most are detected incidentally in asymptomatic patients.
Histologically, they are characterized by the presence of clear cells with abundant intracytoplasmic lipids (microscopic fat) separated by fibroglandular tissue. 70% are lipid-rich adenomas (<10HU in NCCT) and 30% are lipid-poor adenomas (20-25HU in NCCT).
1.2) MYELOLIPOMA:
Benign tumors are composed mainly of mature fatty tissue, usually unilateral. They are generally detected incidentally in asymptomatic patients, although they can give symptoms due to hemorrhage or mass effect when they are large.
Histologically, they are characterized by areas of mature adipose tissue interspersed with hematopoietic tissue from the three lineages. They may contain calcifications or microbleeds.
1.3) METASTASES:
They are the most frequent malignant lesions in the adrenal glands, the main primary tumors being lung, breast, colon, melanoma, renal cell carcinoma, and hepatocellular carcinoma. They can be bilateral in up to 50% of the cases.
In cancer patients, the differentiation between metastasis and adenoma can be difficult, since some adrenal metastases may contain intracellular fat, showing radiological findings that are superimposable with lipid-rich adenomas (attenuation<10UH in NCCT). Likewise, hypervascular metastases can present contrast washout rates such as adenomas.
DDX: primary adrenocortical carcinoma(ACC), that has more locoregional invasion than metastasis.
Another less frequent lesion to mention, is the adrenal collision tumor. It is a mass formed by the coexistence of two histologically different adrenal tumors.
1.4) ADRENAL TUBERCULOSIS:
Destruction of the adrenal cortex gland secondary to tuberculosis infection, conditioning adrenal insufficiency.
Radiographic findings depend on the elapsed time of adrenal involvement. CT and MRI features:
- In early stages: bilateral adrenal enlargement with decreased attenuation central, secondary to caseous necrosis.
- In chronic cases: adrenal atrophy with calcifications and irregularity of its contours.
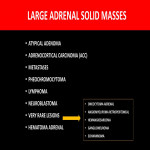
2. LARGE SOLID MASSES
2.1) ATYPICAL ADENOMA:
CT and MRI: may appear as a mass>4cm, heterogeneous with areas of necrosis, hemorrhage, and calcifications. It can present mixed areas with variable attenuation values [<10HU and ≥ 10HU] and heterogeneous drop in signal intensity in the “opposite phase”.
DDX: collision tumor, ACC, metastasis, and pheochromocytoma.
2.2) ADRENOCORTICAL CARCINOMA:
Rare tumors are derived from the adrenal cortex, with a peak impact in childhood and middle age. It can manifest as Cushing's syndrome in hyperfunctioning tumors and/or with abdominal pain, and a palpable mass due to its large size.
Histologically: Neoplastic proliferation of epithelioid cells, with abundant pale-staining lipid-rich cytoplasm, and atypical nuclei, with multiple mitotic images. A relatively rich and delicate vascular supply is present. These cells are negative for neuroendocrine markers.
DDX: large adrenal metastases or neoplasms of the adjacent organs, which invade the adrenal gland, requiring a histological study+/-surgery for its correct diagnosis.
2.3) PHEOCHROMOCYTOMA:
Rare tumor originating in the adrenal medulla. It has been called the "10% tumor":
- 10% bilateral
- 10% extraadrenal
- 10% in children
- 10% associated with syndromes
- 10% malignant
- 10% with calcifications.
The diagnosis is a clinical, laboratory, and radiological.
Histologically: The architectural pattern includes a combination of cell nests and trabeculae. The cytoplasm can be eosinophilic and finely granular.
Some authors nickname it as "the image chameleon" due to its complex and variable appearance which can simulate other lesions. Its diagnosis is suggested by elevated catecholamines in blood/urine.
2.4) LYMPHOMA:
Secondary adrenal lymphomatous involvement is more common than primary adrenal lymphoma, being more frequent due to non-Hodgkin's lymphoma. It is frequently associated with retroperitoneal lymph node disease.
Histologically, a diffuse neoplastic proliferation of medium-large lymphoid cells.
Its radiological characteristics are like other adrenal neoplasms, and its diagnosis is usually suggested by the involvement of other lymph nodes.
2.5) NEUROBLASTOMA:
Most common extracranial solid childhood neoplasm, frequently in adrenal glands. Generally, it is totally asymptomatic, becoming clinically evident when it invades or compresses adjacent structures, metastasizes, or determines a paraneoplastic clinical picture.
This lesion usually presents necrosis and intra-lesional hemorrhage. Calcifications are detected in 80–90% of cases and represent an important finding to differentiate this neoplasm from Wilms tumor.
DDX: Wilms tumor.
2.6) VERY RARE LESIONS:
- A. SARCOMA ADRENAL: Sarcomas primary in the adrenal are rare; two tumors that may occur include angiosarcoma and leiomyosarcoma. For the diagnosis is required a histological study +/- surgery.
- B. ANGIOMYOLIPOMA RETROPERITONEAL: Its radiological findings are like adrenocortical carcinoma.
- C. ONCOCYTOMA: Adrenal oncocytoma is an uncommon benign tumor with about 110 cases reported in the literature and median patient age of 46years. Histopathology: Microscopically, tumors have abundant deeply eosinophilic (mitochondria-rich)cells. As with other adenomas, immunohistochemistry is typically positive for vimentin, melanA, inhibin-α, and calretinin and may be immunoreactive for synaptophysin. They also may be immunoreactive for mitochondrial antigen MTCO2 and variably positive for CK8, CK18, and CD10.
2.7) ADRENAL HEMATOMA:
Adrenal hemorrhage is usually secondary to trauma (80%) however, it can also be the result of anticoagulant therapy, severe stress, or internal bleeding from adrenal lesions.
Post-traumatic hemorrhage usually manifests with abdominal pain, it is usually unilateral, frequently affecting the right adrenal.