Type:
Educational Exhibit
Keywords:
Cardiac, Mediastinum, Thorax, Plain radiographic studies, Arterial access, Catheters, Complications, Cardiac Assist Devices, Haemodynamics / Flow dynamics
Authors:
T. Cobo Ruiz, D. Castanedo Vázquez, D. Herrán de la Gala, P. Menéndez Fernández-Miranda, A. Pérez del Barrio, P. Sanz Bellón, E. Peña Gómez
DOI:
10.26044/ecr2022/C-13256
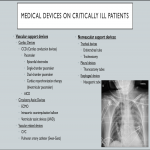
Findings and procedure details
VASCULAR SUPPORT DEVICES:
- Cardiac devices
- CCD (Cardiac conduction devices)
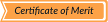
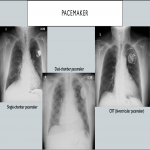
- Pacemaker: A pacemaker is a device that regulates the heart rate using electrical impulses delivered through electrodes to the myocardium. They improve cardiac function, reduce the severity of clinical symptoms, and reduce mortality and morbidity.
- Epicardial electrodes.
- Single-chamber pacemaker.
- Dual-chamber pacemaker.
- Cardiac resynchronization therapy (biventricular pacemaker): CRT usually involves atrial synchronized ventricular pacing to optimize atrioventricular timing with biventricular pacing to promote ventricular synchrony and improve ejection fraction, left ventricular size, and mitral regurgitation.
- Potential complications related to de use of this cardiac conduction device include pneumothorax after its placement, migration of the components, perforation, "Twiddler" syndrome or pacemaker lead fractures.
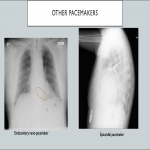
- AICD (automatic implantable cardioverter-defibrillator): This is a common cardiac device designed for both patient monitoring and therapy in case of ventricular tachycardia or fibrillation, capable of producing a large amount of electrical energy in a single output and therefore defibrillating the heart. It is mainly used in patients with tachydysrhythmias and for preventing cardiac arrest. An AICD usually comprises of a single lead with one or two shock coils (with a thick electrode to reduce the risk of damage to the myocardium).
-
- Circulatory Assist Devices:
- ECMO:
- The ECMO system provides oxygenated blood and extracts carbon dioxide. The two main types of ECMO devices are veno-arterial (VA) ECMO and veno-venous (VV) ECMO. Both allow respiratory support, but only VA ECMO allows hemodynamic support.
- In VV ECMO, the femoral cannula tip should be at the junction of the inferior vena cava and the right atrium, and the internal jugular vein cannula tip at the junction of the superior vena cava and the right atrium. Therefore, the oxygenated blood returns to a systemic vein or the right atrium
- Cannulation sites for VA ECMO depend on the device configuration, with femoral-femoral being the most frequent. With VA ECMO, deoxygenated blood is deflected from a vein while oxygenated blood returns to an arterial vessel, providing hemodynamic support.
- Among the complications, misplacement of the ECMO cannula can lead to vessel obstruction or occlusion. Other complications include gas emboli, thrombosis of veins or arteries, cerebral ischemia, stroke and hemorrhage.
- Intraaortic counterpulsation balloon:
- This polyethylene balloon spans the entire length of the thoracic aorta and it's placed percutaneously through femoral artery access. The balloon inflates during diastole increasing blood flow to the coronary arteries, great vessels, and renal arteries. Immediately prior to systole, it deflates producing a vacuum effect that increases blood flow to the aorta and its branches. Although the intraaortic counterpulsation balloon is predominately radiolucent, it has radiopaque tips proximally and distally, and the cranial radiopaque tip should be 2 cm above the carina on the chest radiography.
- Complications related to an intraaortic counterpulsation balloon might be vascular (limb or mesenteric ischemia, renal insufficiency, aortic dissection...) and non-vascular (malposition, infection, neurological complications...)
- Ventricular assist devices:
- Left ventricular assist device (LVAD): The main indication for LVAD is being a bridge to cardiac transplantation. These models consist of a pump that takes blood from the left ventricular apex into the ascending aorta through an outflow cannula connected to a conduit that is anastomosed to the ascending aorta. The conduit is not radiopaque on conventional radiograph (however, it could be visualized on CT).
- Complications of ventricular assist devices include pneumothorax, hemothorax, postoperative hemorrhage, cardiac tamponade, thromboembolism, arrhythmia, or infection, among others.
- Vascular related devices
- Central venous catheter (CVC):
- A central venous catheter provides access for drugs or fluids administration, monitoring central venous or pulmonary artery pressure, saturation, and several interventions. These catheters are usually inserted via the subclavian or internal jugular vein (less frequently using the femoral vein). Its tip should be positioned at or just above the cavoatrial junction, or also two vertebral body levels below the carina.
- There are variants of this type of catheter, such as peripherally inserted central catheter (PICC) or tunneled CVCs for hemodialysis.
- Complications related to these devices include arterial puncture with intra-arterial placement of the catheter, hemorrhage, pneumothorax, hemothorax, arrhythmia, cardiac tamponade, catheter-related thrombus, pulmonary embolism, air embolism, or infection.
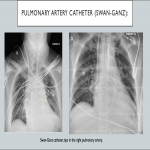
- Pulmonary artery catheter (Swan-Ganz):
- Pulmonary artery catheterization consists of a Swan-Ganz catheter inserted through a central vein (mostly the subclavian or jugular vein) into the right heart and then into the pulmonary artery. It is used to monitor circulatory hemodynamics in critically ill patients by measuring pulmonary capillary wedge pressure (differentiating, for instance, cardiogenic pulmonary edema from noncardiogenic pulmonary edema).
- An ideal location of the tip would be in the right or left pulmonary artery, not extending beyond the proximal interlobar artery, in order to avoid complications such as infarction or pseudoaneurysms.
NONVASCULAR SUPPORT DEVICES:
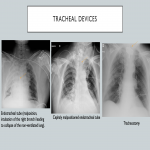
- Tracheal devices
- Endotracheal tube:
- This tube is inserted for maintaining the patency of the airway and to provide airway support. An ideal position for the endotracheal tube tip would be 5 cm above the carina or between the T2 and T4 vertebral bodies, with the patient’s head in a neutral position.
- The most frequent complication related to an endotracheal tube is malposition. A cephalic malpositioned endotracheal tube leads to inefficient ventilation, distension of the stomach, or even vocal cord injury. On the other hand, if the endotracheal tube is located too caudally, the tube can selectively intubate one of the main bronchi (usually the right), leading to segmental or complete collapse of the non-ventilated lung. Accidental intubation of the esophagus is also a potentially fatal complication.
- Tracheostomy:
- Tracheostomy tubes are used in those patients who will require long-term ventilation. Its distal end should be midway between the stoma and the carina, about the level of the third dorsal vertebra. The position of the tracheostomy tube is maintained with neck flexion and extension, the width of the tube should not exceed two-thirds of the tracheal width, and the cuff should not distend the tracheal wall.
- Possible complications: subcutaneous emphysema, hematoma, and pneumomediastinum. Besides, granulation tissue formation and fibrosis at the site of the stoma can lead to long-term tracheal stenosis.
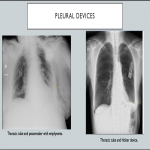
- Pleural devices:
- Thoracostomy tubes:
- Thoracostomy is a common procedure used to evacuate fluid or air from the pleural space. The tip of the tube should ideally be located apically for a pneumothorax evacuation, basally in case of fluid drainage, or in a certain specific location in case of located fluid.
- Some of the complications related to its use include incorrect placement, hematoma, kinking, tube blockage or occlusion, and reexpansion pulmonary edema.
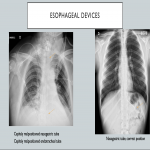
- Esophageal devices:
- Nasogastric tube:
- Nasogastric tubes are frequently used for feeding and administration of medication, but also for suction of stomach contents. This tube has a thin radiopaque marker line along one side, useful to be identified in chest radiography. The tip of the nasogastric tube would be ideally located in the stomach caudal to gastric cardia, or at least 10 cm distal to the gastroesophageal junction.
- Malposition of the nasogastric tube is one of the commonest complications, and it can lead to more severe complications such as lung perforation, esophageal perforation, bronchoaspiration, pneumonia, and pneumothorax.