Hemoperitoneum on CT - main findings and signs
Fluid density and configuration
One can distinguish free intraperitoneal fluid from hemoperitoneum by measuring the fluid density. On unenhanced images, unclotted blood is hyperdense (around 30-45 HU), compared to simple free fluid (< 15 HU), due to its high protein content. In the first few hours of hemorrhage, as blood begins to clot, the density increases (HU > 60), with geographic areas of high density surrounded by areas of low density. [1,2]
With time and progressive lysis of hemoglobin, the blood decreases in size and density. [2]
It is important to note that these values can be lower in individuals with decreased serum hematocrit levels. [1]
The configuration of free fluid can also help pinpoint the origin of the bleeding. Typically, triangular shape interloop fluid collections are classically associated with mesenteric or bowel hemorrhage [1].
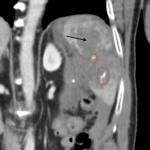
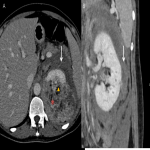
Sentinel clot sign and active extravasation
As bleeding starts, clots tend to from near the site of bleeding. Therefore, the identification of an heterogeneous and hyperdense clot allows localization of the bleeding site (sentinel clot sign). [2]
An extremely important feature to look for is active extravasation of intravenous contrast. It presents as hyperdense foci, isodense to the nearby vessels, indicating active bleeding. It can appear as a serpiginous high-attenuation area surrounded by a large hematoma. [1,2]
The presence of active extravasation is indication for emergent treatment (either embolization or surgery). [1]
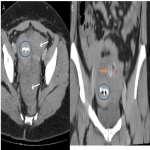
Peritoneal recesses
Another aspect to be aware of is the peritoneal anatomy and its recesses and where to look for intra-peritoneal fluid if there is clinical suspicion of a solid organ injury. The most dependent portions of the abdominal cavity, in the supine position, are the hepatorenal fossa (Morison pouch) and the pelvic cul-de-sac (either the pouch of Douglas/rectovaginal pouch in women or rectovesical pouch in men). Intra-peritoneal bleeding starts near the organ/structure and travels through expected anatomic pathways. For example, blood from an hepatic hemorrhage will travel from the perihepatic space and hepatorenal fossa, along the right paracolic gutter to the pelvic cul-de-sac. Similarly, splenic hemorrhage will flow from the perisplenic spaces, along the left paracolic gutter, to the pelvis. [1]
Sometimes, a large amount of fluid can accumulate in the pelvis without an obvious hematoma near the injuried organ. Therefore, it is extremely important to always look at the pelvis cul-de-sac and exclude the presence of fluid. [1]
Traumatic Hemoperitoneum
The most common cause of hemoperitoneum is by far traumatic injury to a solid organ, with the spleen being the most frequently injured organ in blunt abdominal trauma (40%), followed by the liver (20%). [1]
However, the liver is the most commonly injured organ when blunt and penetrating trauma happen simultaneously. Usually, the right hepatic lobe is more affected (especially the posterior segment) than the left lobe. [1]
There are several different systems for classifying these solid organ injuries, like the American Association for the Surgery of Trauma (AAST) classification. In some form, all of them categorize them in the same degrees of injury: intraparenchymal contusion, subcapsular hematoma, laceration, fracture and vascular pedicle injury. [1]
Therefore, in the presence of traumatic injury, CT is essential to document the type of injury and its extent, the presence of hemoperitoneum and active extravasation. [1]
Bowel and Mesenteric Injuries
Bowel and mesenteric injuries usually occur together, but can occur separately - purely mesenteric tears can happen in seat-belt-related injuries. [1]
The segments more affected by trauma are the ones more fixed and less mobile, like the terminal ileum and the jejunal portions near the ligament of Treitz. [1]
Most reliable CT signs of small bowel injury:
- Interloop fluid
- Mesenteric hematoma
- Wall thickening with enhancement
- Bowel wall discontinuity
The presence of free air is not a common sign in small bowel perforation, and is less reliable than free fluid, because the intraluminal content of bowel loops consists essentially of fluid. [1]
Nontraumatic Hemoperitoneum
Tumor-associated hemorrhage
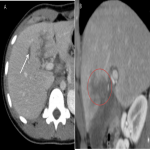
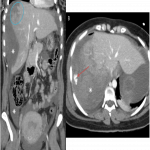
Liver
The most common cause of nontraumatic hepatic hemorrhage is an hypervascular lesion, like hepatocellular carcinoma (HCC) or adenoma. [2]
Hemorrhage due to hepatocellular carcinoma occurs more commonly in Asian countries, where the prevalence of cirrhosis and HCC is also high. It is more common in large peripheral tumors. [1,2]
Rupture of a hepatic adenoma usually occurs in young females with history of oral contraceptive therapy. [1,2]
In these cases, the manifestations can range from minor intrahepatic bleeding or subcapsular hematomas to rupture through the capsule with bleeding into the peritoneum. [1]
On unenhanced CT, the ruptured tumor is hypodense but usually appears obscured by the adjacent hematoma. IV contrast can help identify a ruptured tumor as a large spherical and partially exophytic lesion contiguous with the subcapsular hematoma, and can also help detect active bleeding. [2]
Hemorrhagic metastases are rare, but usually result in massive hemoperitoneum. The most common hemorrhagic metastases are from lung carcinoma, renal cell carcinoma and melanoma. [1]
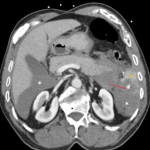
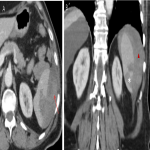
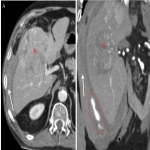
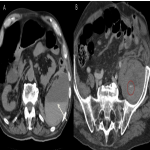
Kidney
Spontaneous hemorrhage into the subcapsular or perinephric space, known as the Wunderlich syndrome, is commonly caused by rupture from a renal tumor, like angiomyolipoma or renal cell carcinoma (RCC). [2]
Sometimes it is difficult to differentiate the mass from the surrounding hematoma, especially in the case of small tumors, and follow-up imaging is advised, after resolution of the hematoma. [2]
The identification of low-attenuation areas of fat within an heterogenous mass is suggestive of an angiomyolipoma. The presence of a solid mass with less contrast enhancement than the adjacent parenchyma points more to RCC. However, this distinction is not always easy. [2]
Gynecologic conditions
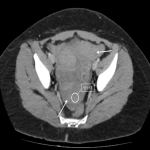
Ruptured ectopic pregnancy
An ectopic pregnancy should be considered in any woman of reproductive age with abdominal pain and elevated serum HCG levels, with absence of intrauterine pregnancy depicted by an ultrasound. [2]
The risk of rupture is severe and can lead to life-threatening bleeding. In the emergency setting, CT will show hemoperitoneum and a ring-enhancing adnexal mass. [2]
Rupture of an ovarian cyst
On the other hand, pelvic pain in a women with negative serum HCG should raise the suspicion of rupture of an ovarian cyst. [2]
CT will show a cystic adnexal lesion with mixed-attenuation (blood mixed with fluid) with associated high-density pelvic hematoma. [2]
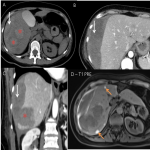
HELLP syndrome
HELLP syndrome is a peripartum condition characterized by a triad of hemolysis, elevated liver enzymes and low platelet count. It should always be considered in pregnant women or women in the imediate post-partum period with acute abdominal pain and laboratory abnormalities. [1]
It can be associated with disseminated intravascular coagulation and other complications, like hepatic hematoma and rupture. [1]
CT is often the modality of choice and shows the presence of subcapsular hematoma or/and hepatic rupture with hemoperitoneum. [1]
Vascular lesions
A ruptured abdominal aortic aneurysm usually results in retroperitoneal hemorrhage, with intraperitoneal hemorrhage being present only in very large leaks that result in bleeding that extends into the peritoneal cavity. [1]
Rupture of a splanchnic artery aneurysm, most commonly the splenic and hepatic arteries, can also lead to hemoperitoneum. In young patients, it should raise the suspicion of systemic vascular disease. [1]
Additionally, vessel erosion by an adjacent inflammatory disorder, like pancreatitis, can also cause hemoperitoneum. [2]
Iatrogenic injuries
Bleeding diatheses is a common complication in patients underdoing anticoagulation therapy. It usually causes hemorrhage into the psoas or rectus muscles, but can also affect the abdominal viscera with perirenal and intramural small bowel hematomas. [2]
On CT, the presence of the hematocrit sign - cellular-fluid level caused by accumulation of cellular elements in the dependent portion of the hematoma - is a sensitive and specific sign of coagulopathy-associated bleeding. [2]
Additoinally, any surgical procedure performed within the peritoneal cavity may be complicated by hemoperitoneum, even the minimally invasive procedures.