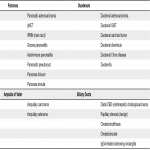
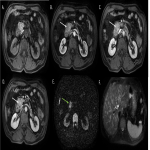
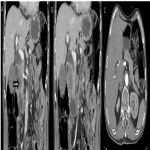
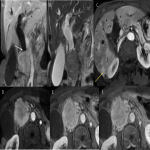
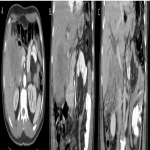
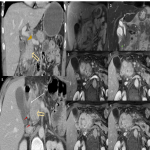
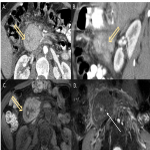
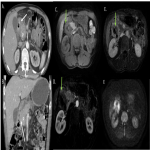
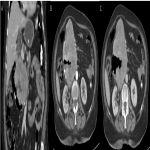
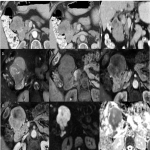
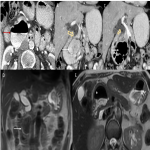
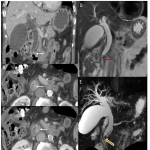
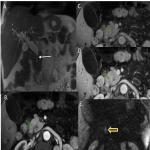
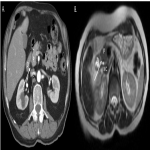
Due to the complex anatomy of the pancreatic groove, it is hard to establish the lesions organ of origin because anatomical structures are located closely and overlap in clinical presentation and imaging features.1,2,4 Figure 2 shows some examples of malignant and benign lesions of this region.
Imaging modalities as Computed Tomography (CT), Magnetic Resonance Imaging (MRI) Magnetic Resonance Cholangiopancreatography (MRCP) may help to distinguish them as the combination of certain clinical and imaging features may suggest a specific diagnosis, preventing the unnecessary burden of additional diagnosis and treatment, even though a histologic confirmation will be required in most cases to discard malignancy.2-5
PANCREAS
PANCREATIC ADENOCARCINOMA
Ductal adenocarcinoma of the pancreatic head sometimes may present as an exophytic mass that appears to arise from the PG;4
- CT and MRI: a heterogeneously enhancing lesion that is hypovascular relative to the normal pancreas with progressive delayed enhancement;1,2
- Typically coexist with pancreatic duct cutoff, ductal obstruction, and upstream pancreatic atrophy;3
- Much more likely to infiltrate posteriorly into the retroperitoneum and encase the adjacent vasculature;3,4,6
- MRCP: double duct sign (if periampullary).1,2
NEUROENDOCRINE PANCREATIC TUMOR (pNET)
Gastrinoma is the most common neuroendocrine tumor occurring at the groove;4
Typical features:
- Circumscribed solid masses hypervascular at CT and MR imaging, demonstrating marked high signal intensity on T2W image;1,4,7,8
- Smaller lesions (< 3 cm) tend to be “functionating” and more homogenous, whereas those unassociated with symptoms tend to be larger and more heterogeneous;1,4,7,8
- Usually displace rather than invade, adjacent structures, although larger masses may have a multinodular border and demonstrate macroscopic invasion;7,8
- Pancreatic duct dilation is uncommon, except in those cases with large masses that obstruct the duct secondary to mass effect;1,8
Atypical features:
- Pedunculated or exophytic lesions that are better visualized on the portal venous phases images compared with the arterial phase;8
Lesions may be cystic, even smaller ones, which typically have a hypervascular rim;1,7
The presence of hypervascular liver metastases can aid the diagnosis.4
GROOVE PANCREATITIS
It is a form of chronic pancreatitis characterized by inflammation and fibrous tissue formation affecting the PG;1-5
Symptoms of biliary or duodenal obstruction are common;3
There are two forms of groove pancreatitis:
- Pure form (involves the groove only between the duodenum and the pancreas) – imaging features consist of loss of fat planes between the head of the pancreas and the duodenum with an ill-defined crescentic frank soft tissue mass;3-5
- Segmental form (affects PG and extends medially into pancreatic head) – this form exhibits a focal hypodense lesion/mass-like enlargement of the pancreatic head close to the duodenal wall;3-5
This soft tissue in the PG has been shown to consist of fibrous scar: it is hypoattenuating at CT, hypointense relative to pancreatic parenchyma on T1WI, and iso- or slightly hyperintense on T2WI, with progressive delayed enhancement;1-5
Other characteristic findings:
- Cystic dystrophy of the duodenal wall (presence of cystic lesions in the thickened duodenal wall);1-5
- Widening distance between ampulla and medial duodenal wall;1-3
- Smooth and regular narrowing of CBD - in contrast to the abrupt and irregular ductal stenosis or complete ductal obstruction seen in patients with pancreatic carcinoma;1-5
- Even in cases of extensive disease, the peripancreatic vessels do not show signs of thrombosis or infiltration.5
The differentiation of groove pancreatitis (especially the segmental form) from pancreatic carcinoma may be difficult, particularly when pancreatic carcinoma has a significant fibrous component.4,5
AUTOIMMUNE PANCREATITIS (AIP)
AIP is a rare benign, IgG4-related, fibroinflammatory form of chronic pancreatitis;1
Diffuse type commonly manifests as a characteristic diffuse enlarged sausage-shaped pancreas with loss of definition of the pancreatic clefts;1,9
Non-diffuse types:
- Focal: typically head and uncinate process, MRI shows a single focal pancreatic mass that may be maybe iso-/hypo-dense to pancreatic tissue and pancreatic duct strictures – mimicking pancreatic adenocarcinoma;9
- Multifocal: evidence of multiple pancreatic masses and multiple pancreatic duct strictures on MRI (highly specific for AIP).9
ANNULAR PANCREAS
It is a rare congenital anomaly in which incomplete rotation of the ventral anlage leads to a segment of the pancreas encircling the second part of the duodenum.2
CT and MRI: evidence of pancreatic tissue and an annular duct encircling the descending duodenum. Pancreatic tissue appears hyperintense on T1WI; T2WI and MRCP can help identify the annular duct surrounding the duodenum.2
DUODENUM
DUODENAL ADENOCARCINOMA
- Adenocarcinomas represent up to 80% to 90% of all primary malignant duodenal tumors and may occur in the periampullary region;4,10,11
- CT and MRI: irregular short-segment concentric/asymmetric thickening of the duodenal wall or intraluminal mass, relatively hypovascular, that results in gradual luminal narrowing;10-12
- Ulceration strongly supports the diagnosis of duodenal adenocarcinoma;2,11
- “Double-duct sign” if periampullary;10
These tumors can be quite difficult to differentiate from groove pancreatitis, especially when they present as focal thickening of the medial duodenal wall.3
DUODENAL GIST
- Duodenal GISTs seem to have a better prognosis than GISTs occurring in the stomach or other small-bowel regions.10 In the duodenum, they are most common in the second portion.8
- Variable appearance on imaging: small GIST appear homogeneous, well-circumscribed endophytic or exophytic mass, whereas large GIST (more frequent) have irregular lobulated margin, heterogeneous enhancement, mucosal ulceration, and central necrosis.1,8,10,11
- Lymphatic involvement and biliary and duodenal obstruction are uncommon, even for large tumors.10,11
When duodenal GIST grows outward exophytically from the duodenum toward the pancreatic head, they are challenging to differentiate from pancreatic head NETs:
- The enhancement level of pancreatic head NET are significantly higher;12
- The size of duodenal GIST is larger, so it presents more often with necrosis or cyst generation;12
- Duodenal GIST often show ulceration, gas, and cavity;11,12
- Biliary obstruction is rare.12
DUODENAL LYMPHOMAS
- Homogeneously and intensely enhancing concentric wall thickening;10
- Not occlusive (gastric outlet obstruction is uncommon);10,11
- Generally have an indolent, slow-growing course;10
- Segmental nodular wall thickening or a large eccentric mass extending into adjacent tissues are typical (producing circumferential wall thickening and irregular “aneurysmal dilatation” of the bowel lumen);10,11
- Splenomegaly and lymphadenopathy in other areas help prospectively raise the diagnosis of lymphoma;10,11
- “Sandwich sign” – the presence of lymph nodes on both sides of the plane of the mesenteric vessels;11
- More common in immunosuppressed patients.10
DUODENAL DIVERTICULUM
- Extraluminal mucosal outpouchings along the medial wall of duodenum within 2-3 cm of the ampulla of Vater;4,11,12
- Incidental finding on CT or MRI, presenting as a round periduodenal structure containing air, fluid, or debris;11,12
- Occasionally can cause complications: nonbiliopancreatic complications include diverticulitis, hemorrhage, perforation or fistula formation; biliopancreatic complications include bile duct stone formation, biliary obstruction, cholangitis, and pancreatitis;2,4
- May mimic other groove diseases such as a tumor or a pancreatic pseudocyst or abscess;4,11
- Lemmel's syndrome - obstructive jaundice from a periampullary duodenal diverticulum.2
AMPULLA OF VATER
AMPULLARY ADENOMA
- Premalignant lesion arising in and around the duodenal papilla;1,2
- Typically asymptomatic and incidentally discovered on endoscopy;1,2
- Ampullary smoothly marginated enhancing mass (> 1 cm);1,2
- Extra-hepatic biliary and pancreatic duct dilation can also be seen.1,2
AMPULLARY CARCINOMA
- A heterogeneous group of malignant epithelial neoplasms arising from the distal biliary epithelium of the ampulla of Vater;1,2
- Generally manifests as an irregular enhancing (not delayed) small mass with lobulated or infiltrative margins at the distal margin of the pancreaticobiliary junction;11,12
- MRCP: typically manifest as a filling defect or focal stricture at the distal end of a dilated CBD;1,11
- Double duct sign (approximately half of cases);1
- Less commonly, the tumor may be undetected by imaging.1,11
The focality of these malignant lesions at the ampulla should be distinguished from the more ill-defined crescentic soft tissue seen with groove pancreatitis.2
COMMON BILIARY DUCT
DISTAL CHOLANGIOCARCINOMA
Cholangiocarcinoma arising from one-third distal CBD account for up to 20% of cases;2
- The key features of this entity are biliary duct dilation terminating abruptly at a point of ductal wall thickening or a polypoid mass;1,2,4
- CT and MRI: both subtypes show biliary dilation with abrupt termination at the mass level and delayed enhancement.1,4