The lymphatic system transports tissue fluid back into blood circulation. Normal lymphatic drainage from the extremities occurs via valveless lymphatic capillaries located in the dermis, which drain to valve-containing lymphatic vessels in the subcutaneous soft tissues, thereafter to deep lymphatic tracts and lymph nodes in regional drainage basins before passing into the lymphatic ducts of the trunk.
Lymphoedema is defined as the chronic, progressive accumulation of lymph in extracellular spaces. It most commonly involves the lower limbs and genitals, but may also affect the upper limbs or head/neck. The chronic stasis of protein-rich lymph results in limb swelling due to a combination of oedema, inflammation, adipose deposition and tissue fibrosis. The associated immune dysregulation leads to increased susceptibility to infection [1].
Lymphoedema may be primary or secondary. The latter is much more common, typically iatrogenic, or following trauma or infection. The most common causes of secondary lymphoedema in the developed world is prior lymph node dissection or radiotherapy in cancer treatment. In the developing world, the most common cause of secondary lymphoedema is parasitic worm infection (filariasis)[10].
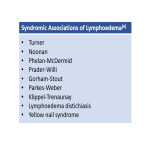
Primary lymphoedema, in contrast, is rare. It arises from anatomical or functional developmental disorder of the lymphatic system. Primary lymphoedema may present at any time from birth, childhood/adolescence to adult life, typically manifesting by 35 years of age[2,3]. The current hypothesis is that most cases of primary lymphoedema have a genetic origin, although a causative mutation is identified in only 1/3rd of affected individuals[6]. Primary lymphoedema may be sporadic (presumed de novo mutations), familial non-syndromic (lymphoedema also in a first degree relative) or it may present as part of a recognised syndrome.
Mutations in least 31 genes or loci have been identified in patients with primary lymphoedema
[6].
The psychosocial morbidity and reduced quality of life caused by chronic lymphoedema typically outweighs the clinical burden of disease. Receiving a diagnosis of lymphoedema is often a source of relief for patients. However, the heterogeneous phenotype of primary lymphoedema poses a diagnostic challenge to clinicians. Many other causes of lower limb swelling mimic lymphoedema: obesity (including lipoedema spectrum); venous insufficiency or deep vein thrombosis; cardiac, renal or liver failure; systemic disease (such as anaemia or hypoalbuminaemia); and medications (amlodipine).
Radionuclide lymphoscintigraphy has long been the mainstay of imaging in patients with suspected primary lymphoedema[4], affording qualitative and quantitative assessment of lymphatic drainage in the upper and lower limbs.