ANATOMY:
The ulnar nerve originates from the C8 and T1 roots.
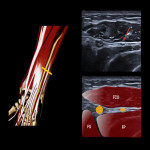
Axilla: in the axilla it is placed between the axillary artery and the axillary vein to later run posteromedial to the brachial artery and median nerve in the arm.
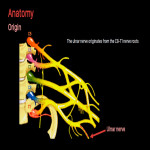
Arm: it then continues down the arm located medial to the vastus medialis of the triceps. In the distal third of the arm it perforates the medial intermuscular septum and becomes more posterior.
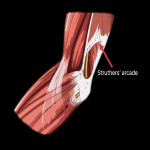
Approximately 6-10 cm proximal to the epitrochlea or medial epicondyle, there is an anatomical structure called the arcade of Struthers which is made up by fibrous bands that form an arcade from the medial intermuscular septum to the triceps fascia, which may favor nerve compression.
The ulnar nerve does not give off secondary branches at this level.
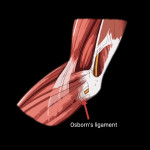
Elbow: the nerve goes down to the elbow region, just behind the epitrochlea to finally enter the epitrochlear-olecranon canal. This osteofibrous canal is formed by the epitrochlea, the olecranon, the retinaculum and the posterior band of the medial collateral ligament.
It continues down the forearm, entering below the arcuate ligament of Osborne, which is a fascia that connects the humeral and ulnar heads of the flexor carpi ulnaris.
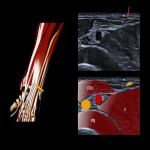
Forearm: afterwards, it continues distally below the flexor carpi ulnaris and between the flexor digitorum superficialis and profundus. At this point, it gives off motor branches to the flexor carpi ulnaris and the medial part of the flexor digitorum profundus (4th and 5th fingers).
Moreover, during this segment, the ulnar artery is positioned laterally to the ulnar nerve to form the neurovascular bundle, which will run distally until it reaches the Guyon's canal.
At the distal exit of the flexor carpi ulnaris there is another potentially compressive fascial structure, the flexopronator fascia. It is made up of interdigitations between the deep fascia of the flexor carpi ulnaris and the fascia of the flexor digitorum profundus and superficialis.
Before reaching the wrist, the ulnar nerve gives off two branches:
1. Dorsal cutaneous branch: it is located approximately 5 cm proximal from the wrist and provides sensory innervation to the dorso-ulnar aspect of the hand and dorsum of the 5th finger and ulnar half of the 4th finger up to the proximal interphalangeal joint.
2. Palmar branch: inconstant branch located at the level of the pronator quadratus. It provides sensory innervation to the hypothenar eminence.
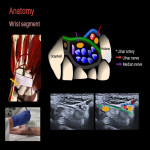
Wrist: in the wrist, it is located inside the Guyon's canal, which is an osteofibrotic canal formed by the pisiform, the hook of the hamate and the Guyon's ligament, and is formed by an extension of the most superficial fibers of the flexor retinaculum.
Distal to the Guyon's canal it gives off two branches:
1. Superficial or sensitive branch: it runs immediately below the Guyon's ligament to later divide into two other small branches.
- Medial branch: that gives rise to the collateral medial nerve of the 5th finger
- Lateral branch: that divides into two other small branches that give off the collateral lateral nerve of the 5th finger and ulnar collateral nerve of the 4th finger
In addition, from each collateral nerve emerges the dorsal recurrent branch that gives sensation to the back of the finger from the proximal interphalangeal to the tip of the finger.
2. Deep or motor branch: it runs deep to the Guyon's canal, below the abductor digiti minimi muscle, describing an arc across the hand from medial to lateral, running deep to the flexor tendons and over the aponeurosis of the volar interosseous muscles.
Along this journey, it gives off the motor branches for the hypothenar musculature, two muscles of the thenar musculature (the deep head of the flexor pollicis brevis and the adductor pollicis), the 3rd and 4th lumbricals and the interosseous muscles.
It is very important to know the innervation field of each branch of the ulnar nerve in order to understand the semiology of the ulnar nerve pathology.
PATHOLOGY:
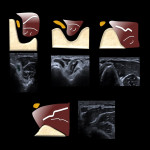
In order to evaluate the different pathologies of the ulnar nerve we must perform a static study and, occasionally, dynamic maneuvers. The static study must be carried out in the axial plane, to detect the existence of fascicular edema, and in the longitudinal plane to detect the existence of caliber changes.
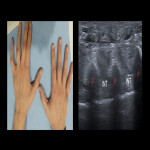
The symptoms related to ulnar nerve injury are medial elbow pain with a positive Tinel sign, paresthesias and numbing on the ulnar side of the forearm and hand (4th and 5th fingers), and progressive weakness of the hand with atrophy of the interosseous muscles and hypothenar eminence.
This can lead to an inability to separate the fingers as well as to a "claw hand" (hyperextension of the metacarpophalangeals and flexion of the interphalangeals). A positive Froment sign can also be found.
1. Entrapment nerve syndromes: chronic irritation is believed to interfere with the perineural and intraneural microvasculature. Ischemia due to compression of the vasa nervorum and venous congestion results in fascicular edema. Progression to a more chronic stage results in fibrotic changes in the nerve sheath (perineural fibrosis).
On ultrasound, we can see diffuse or focal nerve enlargement with loss of its typical honeycomb pattern and hypervascularization on color Doppler.
- Anatomic variants:
- Struthers arcade, Osborn's ligament, flexopronator fascia. Although the Struthers arcade and the flexopronator fascia are insufficient to produce a complete compression of the nerve, it could be the origin of partial improvements after decompression surgeries of the Osborn's ligament.
- Epitrochlear or accessory anconeus: inconstant muscle located between the retinaculum and the skin and found in approximately 5-10% of the population. Its contractile capacity makes it a structure potentially capable of compressing the ulnar nerve.
- Accesory abductor digiti minimi: inconstant muscle located above the neurovascular structures of the Guyon's canal, found in approximately 30% of the population.
- Bone alterations: fractures, osteophytes, loose bodies or heterotopic ossifications.
- Joint alterations: ganglion cysts or pannus
- Vascular alterations: ulnar artery pseudoaneurysms or/and thrombosis
2. Nerve instability: the posterior band of the medial collateral ligament and the retinaculum are tensed with elbow flexion. If the retinaculum is present the nerve is stable and is compressed between the two structures in extreme flexion. If not, the nerve slides over the epitrochlea.
Moreover, there are anatomical variants in the triceps that predispose to dislocation, such as the low insertion of the vastus medialis.
3. Tumors:
- Schwannoma: primary neural tumors of the upper extremity are rare and represent less than 5% of soft-tissue neoplasms of the upper extremity. Among benign peripheral nerve tumors, schwannomas are the most common. They may appear as slow-growing focal swellings that could be painless or not, and that could manifest a positive Tinel sign, paraesthesias and motor weakness. The simple removal of the tumor after careful dissection is generally enough since the recurrence and malignant transformation rates are low.
4. Trauma:
There are different types of traumatic injuries:
According to its severity:
- Neuropraxia: focal demyelination but with preservation of intact axons. In this case, the ultrasound is normal.
- Axonotmesis: axonal damage and Wallerian degeneration with intact perineural connective tissue.
- Neurotmesis: complete disruption of the nerve.
According to its cause:
- Elongation and contusions: the nerve manifests on ultrasound as a wavy hypoechogenic structure with fusiform enlargement. Lacerations could be found. It may be caused by the contact of the nerve with bony surfaces or surgical material in places with little mobility.
- Laceration: it could be a complete disruption, which creates an end-bulb neuroma, or a partial disruption which leads to a neuroma-in-continuity.
- Foreign bodies:
5. Post-surgical changes
Partial lacerations are usually treated with neurolysis while complete lacerations could be treated with end-to-end anastomosis or with the interposition of nerve grafts or neurotubes, depending on the size of the gap.