Normal Imaging Findings
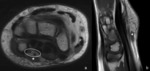
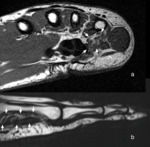
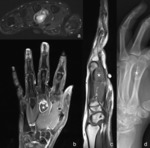
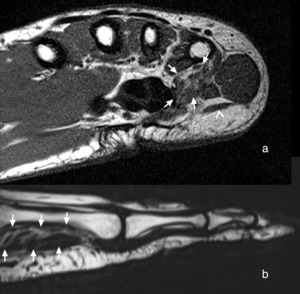
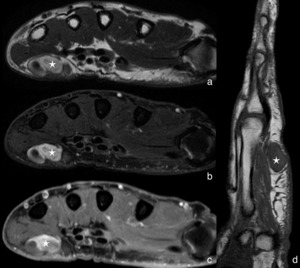
Normal MR imaging appearance of the intrinsic muscles of the hand is not different from the appearance of other skeletal muscles.
On non fat suppressed T1,
T2 and intermediate weighted MR images,
muscles are typically intermediate intense compared with the hyperintense signal of fat or the hypointense signal of cortical bone.
On fat suppressed T1,
T2 and intermediate weighted images,
muscles typically appear hypointense as compared to cartilage or joint fluid on T2 weighted sequences.
Other than at larger extremities as for example the thigh,
the frequent lack of intercalated fat layers makes it more difficult to discriminate the individual muscles of the hand from each other,
especially for the hypothenar and thenar muscles,
where partial volume artifacts due to the oblique course of the muscles impede muscle discrimination additionally.
Because of the small size of the intrinisic muscles of the hand,
high resolution imaging is needed for correct assessment,
preferredly with an in-plane resolution of 0.5 to 1.0 mm and a slice thickness equal or smaller than 3 mm.
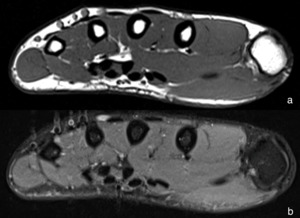
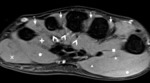
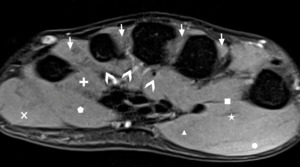
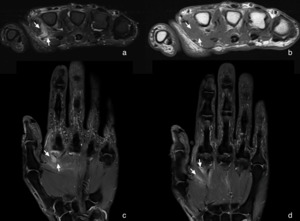
Fig. 1: Axial intermediate weighted MR images of normal appearing intrinsic muscles of the hand without (a) and with (b) fat suppression.
Function and Anatomy
The motion of the hand is enabled by the complex interaction of intrinsic and extrinsic muscles,
which originate and insert within the hand itself (intrinsic muscles),
or originate essentially in the forearm before inserting within the hand (extrinsic muscles).
The extrinsic muscles are not covered in this poster.
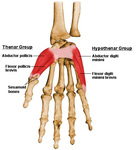
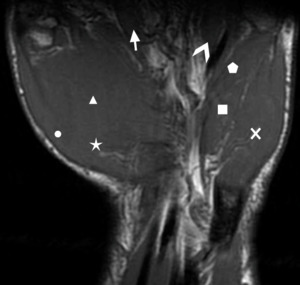
The intrinsic muscles comprise the thenar and hypothenar muscles (Fig. 2, Fig. 3),
which control the motion of the thumb and little finger,
respectiveley.
The interosseous (Fig. 4,
Fig. 5) and lumbrical muscles are also part of the intrinsic muscles and exert their effect on almost all fingers of the hand.
Thenar Muscles:
|
Flexor Pollicis Brevis Muscle (Fig. 2, Fig. 6)
|
|
The flexor pollicis brevis muscle's main function is flexing the thumb,
but it also assists in turning the thumb toward the other fingers at the end of flexion.
The flexor pollicis longus tendon runs through a muscular groove of the flexor pollicis brevis muscle.
|
|
Innervation: Deep branch of the ulnar nerve (deep head of the muscle) and terminal branches of the median nerve (superficial head of the muscle)
Blood supply: Superficial palmar branch of the radial artery
Origin:
Superficial head: volar tubercle of the trapezium and distal lateral border of the volar transverse carpal ligament
Deep head: trapezoid and capitate bone,
floor of the carpal tunnel
Insertion: Lateral tubercle and lateral sesamoid of the volar plate of the thumb at the base of the proximal phalanx
|
|
Abductor Pollicis Brevis Muscle (Fig. 2, Fig. 6, Fig. 7)
|
|
The abductor pollicis brevis muscle is the most superficial thenar muscle and abducts the thumb into a right angle to the palm.
|
|
Innervation: Recurring branch of the median nerve
Blood supply: Superficial palmar branch of the radial artery
Origin: Flexor retinaculum,
palmar surface of the trapezium and scaphoid bone
Insertion: Base of the proximal phalanx of the thumb (and optionally on the lateral aspect of the joint capsule and dorsal aponeurosis)
|
|
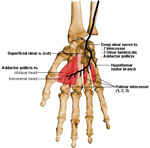
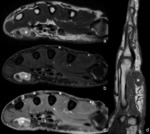
Adductor Pollicis Muscle (Fig. 4, Fig. 6)
|
|
The adductor pollicis muscles enables the unique feature of the thumb to oppose the other fingers by adducting the thumb.
It is triangular in shape,
typically comprises two heads,
and is the deepest thenar muscle.
The two heads form the adductor-interosseous compartment,
passage for the radial artery (which forms the deep palmar arch).
|
|
Innervation: Deep branch of the ulnar nerve
Blood supply: Deep palmar arterial arch
Origin:
Transverse (1st) head: Palmar crest of the third metacarpal bone
Oblique (2nd) head: Capitate bone,
palmbar base of the second and third metacarpal bones,
dorsal carpal ligaments
Insertion: Base of the proximal phalanx of the thumb (including the ulnar-sided expansion of the dorsal aponeurosis,
ulnar tubercle and ulnar-sided sesamoid)
|
|
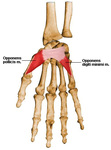
Opponens Pollicis Muscle (Fig. 3,
Fig. 6, Fig. 7)
|
|
By pulling the thumb forward and medially (in a rotational movement),
the opponens pollicis muscle acts as a synergistic muscle to the abductor pollicis muscle,
when opposing the thumb to the other fingers.
|
|
Innervation: Recurring branch of the median nerve
Blood supply: Superficial palmar branch of the radial artery
Origin: Palmar crest of the trapezium bone,
flexor retinaculum,
capsule of the first metacarophalangeal joint
Insertion: Radial side of the first metacarpal bone
|
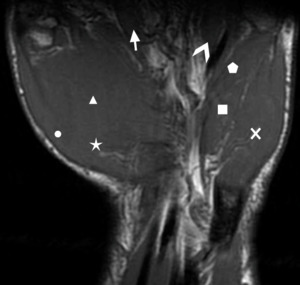
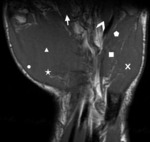
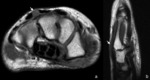
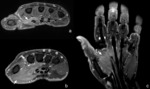
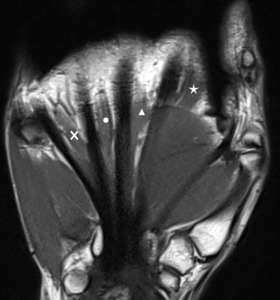
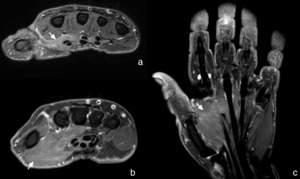
Fig. 7: Coronal T1 weighted MR image with abductor pollicis brevis (circle), flexor pollicis brevis (triangle), opponens pollicis (asterix), 1st (arrow) and 4th (arrowhead) lumbrical, flexor digiti minimi (rectangle), opponens digiti minimi (pentagon) and abductor digiti minimi (cross) muscle.
Hypothenar Muscles:
|
Abductor Digiti Minimi Muscle (Fig. 2, Fig. 6, Fig. 7)
|
|
Similar to the dorsal interosseous muscles at the other fingers,
the abductor digiti minimi muscle abducts the little finger away from the other fingers.
It is the most variable hypothenar muscle and might also be absent in some cases.
Ocassionaly it may also be joined by accessory tendon slips of the flexor carpi ulnaris muscle or palmaris longus muscle.
It may also insert on the sixth metacarpal bone in cases of polydactily.
|
|
Innervation: Deep branch of the ulnar nerve
Blood supply: Ulnar artery
Origin: Pisiform bone,
flexor carpi ulnaris tendon,
pisohamate ligament
Insertion: Ulnar-sided base of the proximal phalanx of the little finger,
including the metacarpophalangeal joint capsule and aponeurosis of the extensor digiti minimi muscle
|
|
Flexor Digiti Minimi Muscle (Fig. 2, Fig. 6, Fig. 7)
|
|
The flexor digiti minimi muscle mainly flexes and slightly adducts the little finger in the carpometacarpal and metacarophalangeal joint.
|
|
Innervation: Deep branch of the ulnar nerve
Blood supply: Ulnar artery
Origin: Hook of hamate bone,
flexor retinaculum
Insertion: Ulnar-sided base of the proximal phalanx of the little finger,
including the capsule of the proximal interphalangeal joint
|
|
Opponens Digiti Minimi Muscle (Fig. 3, Fig. 6, Fig. 7)
|
|
Flexing and rotation the fifth metacarpal bone about the carpometacarpal joint is the main function of opponens digiti minimi muscle,
which allows it to oppose the little finger toward the thumb.
|
|
Innervation: Deep branch of the ulnar nerve
Blood supply: Ulnar artery
Origin: Hook of hamate bone,
flexor retinaculum
Insertion: ulnar-sided shaft of the fifth metacarpal bone
|
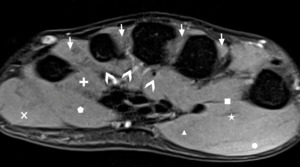
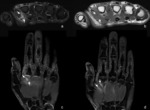
Fig. 6: Axial fat suppressed intermediate weighted MR image with abductor digiti minimi (cross), flexor digiti minimi (pentagon), opponens digiti minimi (plus), flexor pollicis brevis (triangle), adductor pollicis (rectangle), opponens pollicis (asterix) and abdcutor pollicis brevis (circle) muscle, as well as 1st to 4th dorsal (arrows) and 1st to 3rd palmar (arrowheads) interosseous muscles. Note the difficulty to distinguish thenar and hypothenar muscles due to their oblique course and lack of fat planes, the latter being also worse to recognize on fat suppressed MR images.
Interosseous Muscles:
|
Dorsal Interosseous Muscles (Fig. 5,
Fig. 6, Fig. 8)
|
|
The four dorsal interosseous muscles provide abduction (from the midline) of the index,
middle and ring finger and also serve as additional lateral stabilizers in the metacarpophalangeal joints.
The also assist the lumbrical muscle to flex metacarpophalangeal joints and to extend interphalangeal joints.
There is no dorsal interosseous muscle at the little finger.
|
|
Innervation: Deep branch of the ulnar nerve
Blood supply: Palmar and dorsal interosseous artery
Origin: Bipenate origin at the adjacent metacarpal bones of the index,
middle and ring finger
Insertion:
1st and 2nd muscle: extensor expansion on the radial side of the proximal phalanx of the index and middle finger
3rd and 4th muscle: extensor expansion on the ulnar side of the proximal phalanx of the middle and ring finger
|
|
Palmar Interosseous Muscles (Fig. 4, Fig. 6)
|
|
The three dorsal interosseous muscles provide adduction (toward the midline) of the index,
middle and little finger.
They also assist the lumbrical muscles to flex the metacarpophalangeal joints and to extend the interphalangeal joints.
There is no palmar interosseous muscle at the little finger.
|
|
Innervation: Deep branch of the ulnar nerve
Blood supply: Palmar metacarpal artery via deep palmar arch
Origin: Unipennate origin at the base of the metacarpal bone of the index (ulnar sided),
ring and little finger (radial sided),
as well as from the adjacent carpal ligaments.
Insertion: Tendinous insertion palmar to the axis of the metacarpals at the lateral extensor expansion of the proximal phalanx of the index,
ring and little finger
|

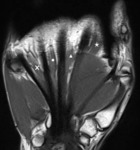
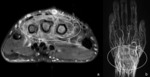
Fig. 8: Coronal intermediate weighted MR image with 1st (asterix), 2nd (triangle), 3rd (circle) and 4th (cross) dorsal interosseous muscle.
Lumbrical Muscles:
|
Lumbrical Muscles (Fig. 7, Fig. 9)
|
|
The full function of the four lumbrical muscles is not yet understood.
Due to their origin at the flexor tendon surface,
they show varying location depending on the contraction state of the flexor digitorum profundus muscle.
They help extending the interphalangeal joint by pulling the flexor digitorum profundus tendons proximally and it is also thought that the lumbricals help flexing the metacarpophalangeal joint when the interphalangeal joints are in extension.
They might also contribute to the radial deviation and abduction of fingers.
|
|
Innervation:
1st and 2nd muscle: Median nerve
3rd and 4th muscle: Deep branch of the ulnar nerve
Variation: 20% of individuals show only innervation of the 1st muscle by the median nerve,
and another 20% of individuals show innervation of the 1st,
2nd,
and 3rd muscle by the median nerve.
Blood supply: Superficial palmar arch,
common palmar digital artery,
deep palmar arch,
and dorsal digital arteries
Origin: Unipennate (1st and 2nd muscle) and bipennate (3rd and 4th muscle) origin at the palmoradial surface of the flexor tendons at the level of the wrist and proximal palm
Insertion: Extensor expansion distal to the metacarpophalangeal joint (distally to the insertion of the interosseous muscles)
|
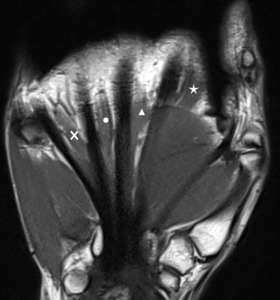
Fig. 9: Coronal intermediate weighted MR image with 1st (asterix), 2nd (triangle), 3rd (circle) and 4th (cross) lumbrical muscle.
Spectrum of Abnormal Imaging Findings
Abnormal MR imaging muscle substance appearances include increased signal intensity on T2 and intermediate weighted MR images in acute and subacute stages. Fat suppression typically enhances the increase of T2 signal and is therefore recommended for standard MR protocols.
Increased muscle signal intensity on T1 weighted MR images is present if fatty infiltration occured in chronic stages of disease.
Because of natural variation in normal volume of the intrinsic muscles of the hand,
contralateral imaging can sometimes help to judge the amount of atrophy if no other signs of disease are present.
Signal increase on contrast enhanced fat suppressed T1 weighted MR images can raise the diagnostic confidence when small and/or discrete signal abnormalities in fat suppressed T2 or intermediate weighted MR images have to be assessed.
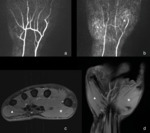
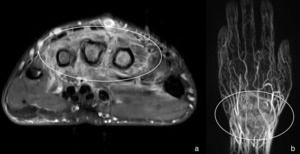
Equally,
time-resolved three-dimensional MR angiogram may help reveal perfusion of pathologic processes and of course tumor vessels when dealing with neoplasia.
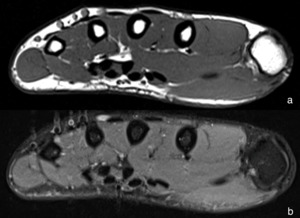
Anatomical Variations:
The presumably most common anatomical variation in the muscles of the hand is an Accessory Abdcutor Digiti Minimi Muscle (Fig. 10,
Fig. 16),
which arises from the flexor retinaculum and inserts at the ulnar-sided base of the proximal phalanx of the little finger together with the normal abdcutor digiti minimi muscle.
It is observed in up to 25% of individuals and hence not very surprisingly is asymptomatic in most of the cases.
But just as other accessory muscles,
it may cause compression of surrounding tissue (particullary the ulnar nerve) and ocassionally causing symptoms in select cases.
It serves as an additonal abductor of the little finger.
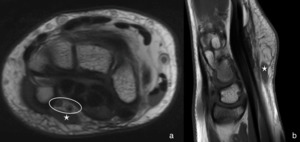
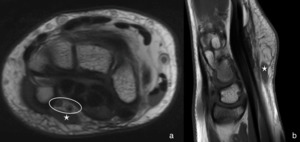
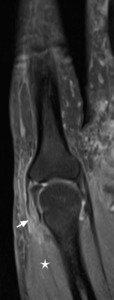
Fig. 10: Axial intermediate weighted (a) and sagittal T1 weighted (b) MR images show accessory abdcutor digiti minimi muscle (asterix), coursing superficial to the ulnar neurovascular bundle (encircled). Incidental finding in a patient subject to imaging for other complaints.
References: RIWAG Radiologisches Institut Weinfelden AG - Weinfelden/CH
The Extensor Digitorum Brevis Manus Muscle (Fig. 11) is a rather uncommon accessory muscle of the hand and is reported to be present in up to 3% of individuals.
It might be uni- or bilateral and originates from the posterior radiocarpal ligament and distal radius.
It most commonly inserts on the extensor hood of the index finger,
but other insertions have been reported as well.
It serves as an additional extensor of the finger.
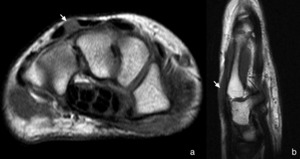
Fig. 11: Axial T1 weighted (a) and sagittal T2 weighted (b) MR images show extensor digitorum brevis manus muscle lying between the extensor tendons of the middle and ring finger. Extensor digitorum brevis manus muscle is an anatomical variant which is more often observed at the ulnar side of the extensor tendon of the index finger, but as also illustrated with this case, shows some variations itself. 13 years old patient was asymptomatic but concerned about the swelling at the back of his wrist.
References: RIWAG Radiologisches Institut Weinfelden AG - Weinfelden/CH
Several other anatomical variations as for example accessory lumbrical muscles,
alternative originis of the lumbrical muscles,
absence of flexor or abductor digiti minimi muscle have been described in the literature and can not be covered in details in this poster.
Except for causing confusing,
they usually are asymptomatic and if exerting deleterious effects,
it is usually due to compression of other anatomic structures (especially in regions with limited space,
as for example in the carpal tunnel).
Other than variation in muscle anatomy itself,
there might also occur some variation in innervation patterns of the intrinsic muscle of the hand.
Trauma- and Exercise-induced Changes:
Like other muscles of the body,
the intrinsic muscles of the hand can be harmed during trauma to the hand.
Injury usually occurs in conjunction with other osseous,
ligamentary and/or tendinous defects and oftentimes will be overlooked because of other prominent findings.
The spectrum encompases the typical features of acute Strains (linear and streaky T2 hyperintense signal changes) (Fig. 12) and complete (discontinuity) or incomplete (partial discontinuity,
volume loss and wavy course) Ruptures (Fig. 13),
which might occur within the muscle substance,
myotendinous junction or at the tendon itself.
Chronic stages of disease are marked with hypointense scar tissue on T2 weighted MR images,
if restitutio ad integrum did not occur.
Atrophy or fatty infiltration may also be present in chronic stages after muscle strain.
Fatty infiltration may be graded according to the Goutallier grading system.
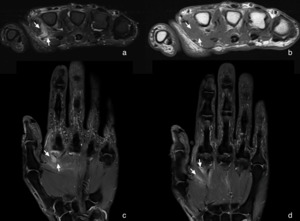
Fig. 12: Axial fat suppressed intermediate weighted (a), axial T1 weighted (b) and coronal fat suppressed intermediate weighted (c, d) MR images show streaky alterations (arrows) within the 1st dorsal interosseous muscle, which proof to be hyperintense only on fluid sensitive sequences (a, c, d) as compared to the hypointense appearence on the T1 weighted sequence (b). Signal abnormalities are consistent with muscle strain in a 61 years old patient who reported a hyperextension trauma.
References: Radiologie am Bahnhof AG - Frauenfeld/CH
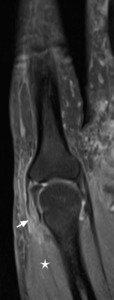
Fig. 13: Coronal fat suppressed intermediate weighted MR image with partial ruptur (arrow) of the 1st dorsal interosseus muscle (asterix) at the myotendinous junction in a 52 years old patient after falling down the stairs. There is accompanying hyperintense muscle edema and wavy course of the myotendinous junction. Intact tendon insertion at the radial sided extensor expansion of the proximal phalanx of the index finger can be appreciated as well.
References: Institut für Radiologie, Kantonsspital Münsterlingen - Münsterlingen/CH
Little is known about exercise-induced signal changes in the MR of the intrinsic muscles of the hand. Although it is known that (excessively) exercised muscle may show a hyperintense signal on T2 weighted MR images compared with non-exercised muscle,
the phenomen of Chronic Exertional Compartment Syndrome and the like have hardly been described for the intrinsic muscles of the hand.
However,
future research with advanced imaging techniques like MR spectroscopy,
T2*-imaging,
arterial spin labeling,
as well as diffusion weighted and perfusion imaging may establish if some not yet completly understood signal changes should be attributed to exercise in certain cases (Fig. 14).
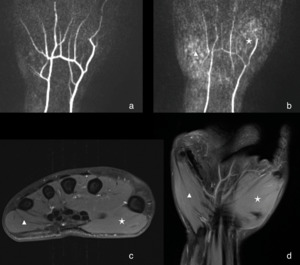
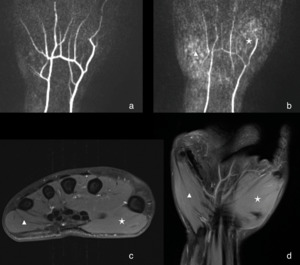
Fig. 14: Time-resolved three-dimensional MR angiogram with perfusion maps (a, b) show increased perfusion at the thenar (asterix) and hypothenar (triangle) eminence without corresponding signal abnormalities in axial contrast enhanced fat suppressed T1 weighted (c) or coronal fat suppressed intermediate weighted MR images. Significance and nature (maybe exercise-indcued changes) remains unknown in 25 years old patient who complained of exertion dependend pain in the hand with radial sided predominance and tenderness on palpation of the second and fourth carpometacarpal joint.
References: Institut für Radiologie, Kantonsspital Münsterlingen - Münsterlingen/CH
Denervation Syndromes:
The intrinsic muscles of the hand are principally innervated from the ulnar and median nerve and hence susceptible to all diseases which might harm these two nerves.
Chronic injuries due to repetitive trauma or compression (Fig. 15) are quite frequent,
especially in areas of limited space like Guyon's canal and the carpal tunnel,
but also acute injury from trauma might disturb normal nerval function and hence cause Muscle Denervation.
Muscle denervation in acute stages causes hyperintense neurogenic edema on T2 weighted MR images,
which can be appreciated within the first days of the causing event.
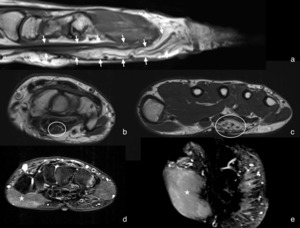
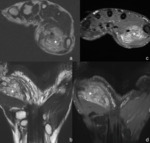
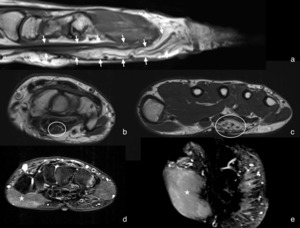
Fig. 15: Sagittal T1 weighted MR image (a) and axial T2 weighted MR images (b, c) show increased perineural fat of the median nerve and increasing enlargement of nerval fascicles (arrows, encircled). On axial (d) and coronal (e) fat suppressed T2 weighted images, faint hyperintense neruogenic edema within thenar muscles (asterix) might be present. 52 year old patient complained of pain at the thenar eminence and carpal tunnel. Imaging and histology was consistent with typical Lipofibromatous Hamartoma of the median nerve.
References: Institut für Radiologie, Kantonsspital Münsterlingen - Münsterlingen/CH
With more longestanding denervation,
atrophy and fatty replacement of the intrinsic muscles of the hand can be shown in chronic stages of disease.
Fatty replacement (Fig. 16) can be graded according to the Goutallier grading system and serves as a prognostic factor for muscle healing potential like for the other skeletal muscles of the body.
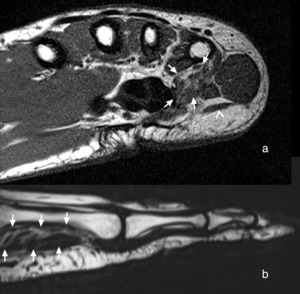
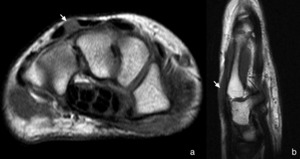
Fig. 16: Axial T1 weighted (a) and sagittal intermediate weighted (b) MR images show fatty infiltration (Goutallier Grade 2-3) of opponens digiti minimi muscle (between arrows). No further investigations for upstream ulnar nerve pathology were attempted since significance of findings was doubtable because 55 years old patient complained only of crepitations at the fourth and fifth extensor tendons.
As another incidental finding, accessory abductor digiti minimi muscle (arrowhead) can be appreciated, as in up to 25% individuals of the normal population.
References: Institut für Radiologie, Kantonsspital Münsterlingen - Münsterlingen/CH
Because of the innervation pattern of the intrinsic muscles and the course of the median and ulnar nerve,
neurogenic edema,
atrophy or fatty infiltration of the thenar muscles typically is sign of compression of the median nerve in Carpal Tunnel Syndrome.
Likewise,
changes of the hypothenar and interosseous muscles are typically suspect for compression of the ulnar nerve in Guyon's canal.
Myositis:
Myositis is an umbrella term encompassing all conditions causing inflammation in muscles.
On (fat suppressed) T2 or intermediate weighted MR images and (fat suppressed) contrast enhanced T1 weighted MR images patchy hyperintense signal change of the muscle substance can be observed.
Distribution of affected muscles usually does not follow innervation patterns and patients present with weakness,
pain,
swelling and sometimes fever and/or elevated laboratory inflammatory markers and sometimes elevated creatine phosphokinase and myoglobin levels.
Myositis may be caused by infection due to skin injuries or sepsis.
Although imaging features of infection are non-specific,
fluid collections and involvement of surrounding tissues should raise suspicion for an infectious origin of disease.
Other causes for myositis include injury,
autoimmune conditions (Fig. 17),
drug side effects,
idiopathic disorders and (as a secondary manifestation) other inflammatory diseases (Fig. 18).
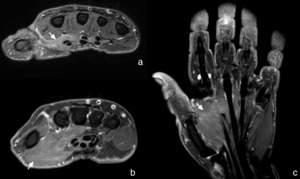
Fig. 17: Axial fat suppressed T2 weighted (a) and axial (b) and coronal (c) contrast enhanced fat suppressed T1 weighted MR images show moderate hyperintense signal increase within the thenar muscles (arrows) in a 49 years old patient with known diabetic cheiroarthropathy and currently restricted movement of the thumb due to pain. Findings were suspect for concomitant Inflammatory Myositis along with the already known Diabetic Cheiroarthropathy.
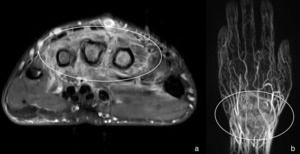
Fig. 18: Axial contrast enhanced fat suppressed T1 weighted MR image (a) shows extensive inflammatory reaction involving both, dorsal and palmar interosseous muscles (encircled), no focal mass could be encountered. Corresponding time-resolved three-dimensional MR angiogram was performed to calculate perfusion maps (b), which show strong synovial enhancement associated with severe synovitis of the wrist (encircled). Although not very suggestiv at imaging, pigmented villonodular synovitis (PVNS) was clinically suspected in this 31 years old patient with massive pain in the dorsal wrist. Incisional biopsy finally proofed Chronic Destructive Synovitis of the Wrist and Extensor Tendons.
References: Institut für Radiologie, Kantonsspital Münsterlingen - Münsterlingen/CH
Complications of myositis include abscesses,
hemorrhage,
compartment syndrome and rhabdomyolysis,
where rapid MR imaging is needed to improve management and prognosis.
Myositis ossificans is a pseudotumor-like,
rarely at the hand occuring condition which is more commonly observed in large muscles.
(Pseudo-) Tumors:
Focal lesions of the hand are commonly observed and often benign.
MR imaging is the key modality to determine the location of lesions of the hand in relation to the surrounding tissues and can help to estimate the nature of lesions.
It hence helps for further management,
peroperative planning or,
in case of malignancy,
local staging of the primary tumor.
However,
MR features of many lesions occuring at the hand are often non-specific. To facilate further management,
it has been proposed to classify lesions as benign,
intermediate grade and malignant,
based on their margins,
enhancement,
bony involvement and other featuers.
Typically Benign Lesions include among others Ganglion Cysts,
Epidermal Cysts,
Fibroma of Tendon Sheath,
Focal Nodular Synovitis,
Nodular Fasciitis,
Lipoma,
Lipofibromatous Hamartoma (Fig. 15),
Hemangioma (Fig. 19),
Hematoma, Bizarre Parosteal Osteochondromatous Proliferation (Fig. 20), Papillary Endothelial Hyperplasia (Fig. 21),
Myositis ossificans,
or Schwannoma.
They usually exhibit smooth or lobulated margins with preseved fat planes,
only rarely cross compartments and show no bony destruction or extensive surrounding reactions.
Often there is no or rim enhancement with no internal enhancement,
but other enhancement patterns can be observed as well.
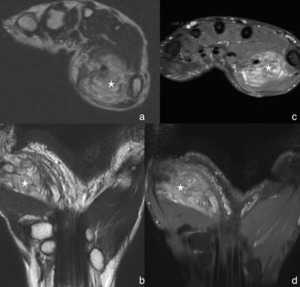
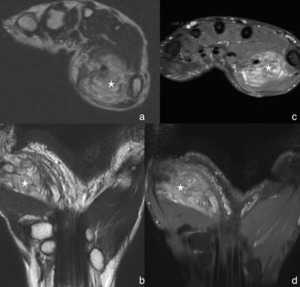
Fig. 19: Axial T1 weighted (a) and coronal T2 weighted (b) MR images show a well-circumscribed lesion (asterix) centered in the opponens pollicis muscle, with inhomogeneous T1 and T2 hyperintense signal. Heterogeneous enhancement of the mass (asterix) can be appreciated on axial (c) and coronal (d) contrast enhanced fat suppressed T1 weighted MR images. 30 years old patient was concerned about the swelling in his wrist at the thenar eminence and otherwise asymptomatic. Histologic result after incisional biopsy was consistent with Hemangioma.

Fig. 20: Axial fat suppressed T2 weighted (a) MR image shows well-circumscribed, inhomogenously hyperintense mass (asterix) palmar to the third metacarpal bone. On coronal contrast enhanced fat suppressed T1 weighted (b) the mass (asterix) shows rim enhancement with some nodular areas, but also with help of the sagittal T1 weighted MR image (c) the location of the mass (asterix) cannot clearly be identified as either intra- (1st palmar interosseous muscle) or extramuscular (bony origin from the metacarpal bone). Oblique radiograph (d) suggested rather extraosseous origin, and intraoperative exploration showed and intermuscular location where the lesion was loosly adjacent to the third metacarpal bone and easily removed. It was finaly histologically proofen as Bbizarre Parosteal Osteochondromatous Proliferation (BPOP), also called Nora lesion. Lesion was an incidental finding in a 35 years old patient who underwent hand x-rays for a history of trauma.
References: Institut für Radiologie, Kantonsspital Münsterlingen - Münsterlingen/CH
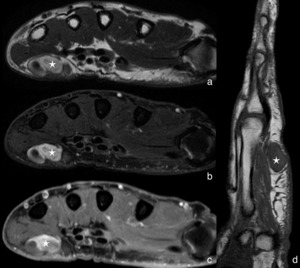
Fig. 21: Axial T2 weighted MR images without (a) and with (b) fat suppression show a well-circumscribed, hyperintense mass (asterix) with some hypointense, rounded foci. Areas with hyperintense signal on T2 weighted images showed also rather homogeneous, avid enhancement on axial contrast enhanced fat suppressed T1 weighted MR images (c). The lesion appeared intermediate intense on sagittal T1 weighted MR images and centered in the subcutaneous tissue of the hypothenar eminence. Giant cell tumor / extraarticular pigmented villonodular synovitis (PVNS) was suspected, but the lesion was histologically identifed as Intravascular Papillary Endothelial Hyperplasia (Masson's Tumor) with thrombosis. 71 years old patient reported growth of the lesion over one year and ocassional acute pain at the hypothenar eminence. Patient was refered to radiology because an intramuscular tumor (sarcoma) could not be excluded on initial clinical ultrasound.
Intermediate Grade Lesions (which are histologically benign but grow locally aggressive) include among others Neurofibroma,
Desmoplastic Fibroblastoma,
Giant Cell Tumor, or Glomus Tumor.
They often show lobulated or even smooth margins but can cross compartments or involve adjacent structures.
Enhancement is often avid,
but rather homogeneous.
Malignant Lesions include among other entities Undifferentiated Pleomorphic Sarcoma,
Squamous Cell Carcinoma,
or Fibrosarcoma.
They usually show irregular,
infiltrative and only rarely well defined margins,
usually cross and invade compartments and adjacent structures and show heterogeneous enhancement patterns.