First questionnaire was filled and returned by 89% of institutions, 69% returned filled data collection sheets for collecting data on imaging parameters for plain radiography and 33% for CT. In total, data on imaging parameters were collected for 255 patients in case of plain radiography and 110 in case of CT. One of the hospitals which didn’t provide data on CT imaging parameters explained that they perform only plain radiography procedures in case of children and although CT unit is available, in case of need for CT imaging, children are sent to nearest university hospital centre.
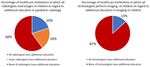
Based on information provided in questionnaires, children are imaged in all healthcare institutions which participated in the survey including children under the age of one year, except in one institution. In most institutions (94%) imaging is performed by all employed technologists and images are read by all employed radiologists while in most of them without appropriate additional education (Figure 1).
In most institutions imaging is performed in the environment which is not child-friendly or is partially adjusted to children’s needs (Figure 2).
In the justification process of medical exposure of a child, both, referrer and radiologist are involved in 63% of healthcare institutions, final decision is made by radiologist in 19% of them and by referrer in 19%. Number of contrast studies of gastrointestinal tract involving use of ionising radiation is significantly reduced in all healthcare institutions in which contrast studies are performed due to the availability and use of ultrasound units. Ionising radiation is sometimes still used for indications which do not imply it as the first diagnostic choice, even though other non-ionising imaging modalities are available (Figure 3). MRI unit is available in 50% of healthcare institutions.
In the majority of institutions (75%) the needs of children are recognised during equipment procurement. Although 69 % of institutions reported that dedicated children imaging protocols exists and are in use, various practices are observed among these hospitals and even within the same hospital (Figure 4).
Gonadal shielding was always used, regardless of body part imaged, use of AEC and recent recommendations [5,7,8]. Careful beam collimation is strongly recommended [3,5,9,10] but in some institutions same collimation was used for children of different ages and sizes. Also, in some institutions use of AEC in case of children of all ages, including those who are under the age of one year was observed while recommendations call for caution regarding the use of it [3,5].
In only two institutions DRLs are established and in only one of them medical physics expert is available.
Based on the first results of the survey, it may be concluded that more attention should be paid to imaging of children in Croatia, including education, child-friendly environment, justification and use of imaging protocols as well as involvement of medical physics expert. More data on imaging parameters are needed in order to set up typical doses for each hospital and then to compare them with the EU paediatric DRLs as a tool for further optimisation, since Croatia still doesn’t have their own national paediatric DRLs.


![Fig. 4: Comparison of typical head CTDI and DLP for two different CT units used in the same hospital. Typical CTDI and DLP values are compared with EU DRL (a) and with some other countries (b) [6]](https://epos.myesr.org/posterimage/esr/eurosafeimaging2020/156341/media/883782?maxheight=150&maxwidth=150)
