Institution
As the largest provider of health services in Turkey, the Ministry of Health is segmented into multiple hospital regions including the Northern Healthcare Region of Istanbul Province (a.k.a. Anatolia North, which consists of 13 hospitals and 6 dental hospitals/centers. In Anatolia North 3 million residents are being served; 11.1 millions outpatient admissions and 250 thousands surgical operations are being performed annually. The annual number of radiologic procedures in Anatolia North are more than 4 milion and roughly represents 1/1.000th of world radiological services.
Umraniye Children’s Hospital is a mid-size receiver hospital within Northern region. Although it is serving to a core population of circa 1.000.000, many patients from oether hospitals and districs also prefer or are referred to this institution.
Why to Establish a Dose Excellence Center?
Umraniye Children’s Hospital was the first pediatric institution in Turkey, where a comprehensive dose management system was implemented, and modern dose surveillance IT applications were used. FSM was designed to comply with highest standards and provide a framework to assist other centers develop the required dose management infrastructures according to relevant IAEA guidelines (4).
Such center of competence (CoC) was required in order to be utilized as initial host institution for fellows that need to be trained within the Anatolia North, and to be a reference center that other hospitals in Turkey can duplicate in order to develop quality assurance practices. The compliance of the facility with the established criteria was verified through a process of systematic and critical analysis of the quality of radiological services to allow comparison of trainees/observers’ practices of service against established standards of good practice.
Basic Guidelines and Criteria for CoC
The facility fulfills all the guidelines and criteria set by IAEA to establish for regional Centers of Competence for QA/QC in diagnostic and interventional radiology (6). Accordingly, (1) objective of the facility; (2) access to institutional/industry funds for the sustainability; (3) infrastructure, i.e. technical (equipment) resources, inventory control (asset management system), number of examinations and procedures (demand) to correspond to the scope of the facility to be a centre of professional education and training regarding the establishment of quality assurance/quality control in radiology; (4) human resources, and (5) quality processes were set to support the duty explained above).
Key Elements of a Dose Excellence System
Lowering dose requires more than technology. An effective dose management approach requires a wing to wing approach from the justification of the examination
(i.e. performing the appropriate procedure) to the optimization of the exposure (i.e. performing the procedure appropriately) (Figure 2). In that context, basic steps and goals of a dose management strategy are as follows:
· Transforming dose awareness from an act to a habit
· Educate personnel
· Justify high dose examinations
· Standardize protocols and practices
· Optimize protocols and practices
· Communicate message to stakeholders
· Promote best practices and be safe
To meet above mentioned goals FSM (or any CoC) has to have below mentioned infrasturucture and proceses:
1. Access to prior exams: FSM has access to patient’s past radiological exams through national teleradiology system, connectiing oll Turkish hospitals, public and private.
2. Appropriateness: Electronical clinical decision support system, embedded in hospital information to assist referring physicians in selecting the most appropriate exam based on the patient’s clinical presentation. This ensures that patients are referred for the “right” imaging study, prevent over-utilisation of imaging, and will prevent unnecessary exposures.
3. Eqipment quality: All CT equipment shpuld meet XR-29 lower dose criteria. Availability of modern dose reduction algoritms (i.e. statistical iterative reconstruction) is preferred.
4. Standardization: Mapping local imaging procedures with standard procedures to obtain uniform scanning and facilitate data analysis. This step includes the asignement to site protocols a specific ID. (i.e. RadLex v.1.2) In FSM, 65 standartized protocols are currently used. The use of nonstandartized protocols are not permitted, unless clearly justified and only exceptionally. Standardization allows to compare protocols/technologies/radiographers, and assists in tracking of examinations and in making comparisons between same protocols of same CT systems. Development and implementation of standardized imaging has also been shown to lead to better results by means of quality imaging and high patient throughput.
5. Continuous education: (1) Technologists orientation training programs to deliver imaging quality training solutions to contribute the transformation in radiology department to shift technicians autonomy from the individual to the professional level. (2) Technical conferences and workshops to apply advanced capabilities of devices into practice making the full use of the systems.
6. Centrally managing and tracking compliance to standartized imaging protocols: An essential component of protocol management, a feature embedded dose tracking software.
7. Availability of diagnostic reference levels (DRLs): These are values which are usually easy to measure and have a direct link with patient doses. They are therefore established to aid efficient dose management and to optimize patient doses. DRLs should not to be exceeded for standard procedures when good and normal practice is performed. If patient doses are found to exceed consistently the corresponding reference level, investigation and appropriate corrective action should be taken, unless the unusually high doses could be clinically or technically justified. As a part of proper radiation protection program, and according to Radiation Protection 109 (EC 1999), Guidance on Diagnostic Reference Levels (DRLs) for Medical Exposures (5), these levels should be established, have to be revised periodically, and be specific to a country or to a region because published DRLs values from other countries (with potentially different imaging practices and technology) may not be relevant to other countries’ particular circumstances. For Turkey, these levels were not established, and Anatolia North’s median DRLs are generally used to fulfill the gap (see poster no: at ECR 2019). For Anatolia North itself, and for FSM in particular unified pan-European DRLs of our CT service provider, Affidea was initially used. These were determined afer median DRLs published from several European countries (Switzerland, Belgium, Finland, Norway, France, Germany, Poland, UK) from 2010 onwards (6).
8. Dose data acquisition, registry and analysis system: In FSM a commercial software (Dosewatch, GEHC) is being used. This web-based vendor-neutral solution captures, tracks and reports radiation dose directly from the medical devices. It monitors and analyzes high dose alerts and patient cumulative dose, includes quality metrics to assess the technical factors, has data consolidation and statistical analysis tools for protocol optimization and dose reduction by optimizing dose levels. In that system if the DLP or CTDIvol for a scan is equal or more than [median x 2], an alert is triggered. Alert thresholds are moving targets; so as technicians got better, dose thresholds become tighter.
9. Justificaton: Cases for whom overdose alert is triggered had to be justified on the dose tracking software by responsible technician to assist finding root causes of overdoses. These justifications might point to patient-related (e.g. obesity, incooperative movements), technician related (e.g. choosing wrong protocol, por iso-centering), or procedure related (e.g. difficult procedure, over-length scanning) factors.
10. Systematic image quality assessment: FSM has an embedded module in its teleradiology system, allowing radiologists to evaluate the image quality. Quality scores are tracked on-line to maintain balance between low doses and clinically useful image quality.
11. Periodical assessments: Meetings to assess the standartization, justification and optimization goals. These meetings also permit detection and retrospective evaluation of severe over-exposures to be analysed by experts in the presence of responsible technologists.
12. Optimization: Distances of hospital DLPs to the initial DRLs (unified pan- European DRLs) that were determined after published data from several European countries (Switzerland, Belgium, Finland, Norway, France, Germany, Poland, UK) from 2010 onwards (6).
13. Patient education: Posters, banners, booklets and audiovisual materials on dose-awareness to be disseminated at imaging facilities.
14. Creating public awareness: Generated a lot of interest across the Anatolia North, nationally broadcasted through TVs, and found place in social media and national press. This interest has created a dose awareness throughout the country.
15. Internal/indpendent audits: To measure current state, identify process gaps and areas to bring more optimization.
Dose Optimization Achievements
For this presentation, data of last calendar year was used. The sequences were acquired with a 128-slices scanner. All patients were measured for length and weight before the study. Color coded protocols was used where appropriate. This procedure was necessary to calculate size specific dose estimates (SSDE) and to perform size-based CT dose optimization. Conventional dose data (CTDIvol, DLP) and detailed dose information (SSDE, effective dose) were also calculated.
During preoptimization period, all doses were significantly higher than pan-European unified DRLs. Same protocol was used for different purposes; hence unoptimised dose levels (i.e. high median doses with large variability) and inconsistent image quality (as reported by radiologist from IQ feedback module of teleradiology system) were common to observe.
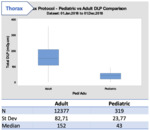
After appropriate trainings and technical optimizations by vendors, physicists and radiologists median and standard deviations improved significantly. Dedicated pediatric protocols enabled healthcare professionals to decrease dose levels drastically for pediatric patients with regard to adult protocols. As an example DLP for thorax protocol was 152±83 for adults (N=12377) , whereas it was only 43±24 for children (N=319) (Figure 4). Dose levels also differed significantly by age group, positively correlating with the body size (Figure 5 and 6).