The increasing incidence of hepatobiliary surgery has also led to an increase in biliary tract injuries and other complications such as biliary leakage. It has been reported that the incidence of biliary injuries after laparoscopic cholecystectomy ranges from 0.2% to 7%, compared to 0.2-0.4% after conventional cholecystectomy [2].
Injuries to the bile tract may result from incorrect bile duct cutting, which can result in leakage, accidentally misplaced clip, and also strictures can be the result of fibrosis or thermal damage [3].
Postoperative bile duct injuries include biliary leakage, stricture, complete cross-section or excision of the bile duct segment, with or without obstruction in the proximal biliary tree due to induced clips; these injuries are classified by Bismuth or Strasberg classification.
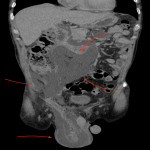
Imaging techniques reveal post-cholecystectomy complications, including biliary extravasation, intra-, and extrahepatic collections, free fluid, cholestasis, and strictures. The various imaging techniques are complementing each other, and no one technique is specific to a particular complication. In patients with pain, fever, jaundice, or bile fistula, the first choice is abdominal US see img 2 and CT see img 3 to assess fluid collections (eg, abscess, biloma) in the upper abdomen [4].
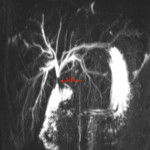
The most accurate imaging method for the complete evaluation of the morphology of bile duct branches is MRCP, see img 4, as it is non-invasive, does not use ionizing radiation, and provides excellent anatomical information about bile duct branching [2, 5].
On the other hand, ERCP, see img 5 provides a therapeutic option if papillotomy and endobiliary stenting can be considered. The ERCP helps identify the location of a bile leak and allows for internal bile drainage if a diagnosis of minor bile duct damage is confirmed. Additional diagnoses, such as cholelithiasis or biliary strictures, can also be treated during the same procedure, so ERCP is now widely recommended as the primary treatment option for postoperative bile leaks [6]. If the ERCP fails, PTHC is the next imaging technique that can accurately visualize the location and nature of the BDI and perform extraluminal percutaneous endoscopic cholangiography with stent insertion to restore bile duct continuity, see img 6 and 7 [7].
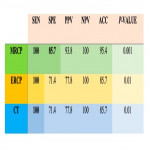
In our study, it was found that the sensitivity of the methods, as well as the specificity and accuracy, depends on the type of biliary damage. MRCP, ERCP, and CT showed 100% sensitivity to type E injuries, which include different types of biliary strictures, however, the specificity and accuracy were higher in MRCP - 85.7% and 95.4%, respectively. In contrast, ERCP and CT showed similar specificity and accuracy for type E lesions in 71.4% and 85.7%, respectively. The superiority of this type of sensitivity and accuracy in MRCP can be explained by the MRCP's improved ability to visualize the anatomical features of the bile ducts, especially if a hepatic-specific contrast agent is used during the study [8].
MRCP and ERCP were superior in non-E-type injuries, including cystic duct leakage with high specificity - 100%, while in this case MRCP also shows high sensitivity (85.7%) and accuracy (95.4%) compared to ERCP, which had slightly lower sensitivity and accuracy, 71.4%, and 85.7%, respectively.