1-CMRI STUDY PROTOCOL:
CMRI tecniques let us a new perspective about the frequency, management, and prognosis of HCM.
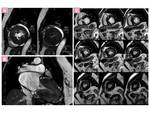
-CINE SSFP MR IMAGING SEQUENCES:
(Cine Steady-state free precession) are used to evaluate:
-Cardiac function measurement
- Biventricular volume quantification and function
- Elevation of left ventricle ejection fraction(LVEF)
- Sistolic disfunction often develops with end-stage HCM.
- Assessment of global and segmental systolic thickening
-Morphological aspects:
- Quantify the Myocardial thickness and mass accurately which are related to the diagnosis and prognosis of HCM:
- Phenotypes:
-
CMRI no limited view is able to define the broad range of phenotypes of HCM Fig. 2, with asymmetric involvement of the interventricular septum being the most common pattern (60-70% of the cases), other variants include apical, symmetric, midventricular, masslike, and noncontiguous HCM.
-
Apical hypertrophic cardiomyopathy (APH) or localized myocardial hypertrophy which can be missed by echocardiography, is easily identified with SSFP
-
Evaluation of recesses, diverticula, aneurysms, clefts, and crypts in genotype-positive and phenotype-negative HCM Fig. 22Fig. 26
-
Anomalíes of Papillary muscle and abnormalities of the tendinous chords Fig. 21Fig. 22 Fig. 25
-
Left atrial size ( and function)
-Pathophysiological components:
-
Contractility anomalies
-
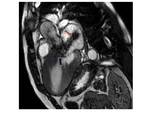
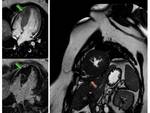
Left ventricle outflow tract obstruction (LVOT) with turbulence jet across the LVOT in patients with asymmetrical septal hypertrophy (ASH) Fig. 9
-
Outflow tract area <2,7cm in systole (100% sensitivity and specificity to differentiate obstructive from nonobstructive HCM) Fig. 4
-
Mitral SAM and mitral regurgitation associated to ASH Fig. 3Fig. 3
-FLOW QUANTIFICATION SEQUENCES. (Velocity-encoded cine MRI, Phase contrast imaging (PC-MRI))
-Direct measurement of outflow tract gradients.
- Dynamic obstruction: instantaneous outflow basal gradient ≥ 30 mm Hg or of ≥50 mm Hg with exercise Fig. 4
-Quantification of concomitant mitral regurgitation
-Diastolic (dys)-function (mitral inflow/pulmonary vein flow)
-LATE GADOLINIUM ENHANCEMENT (LGE)
- T1-weighted Inversion recovery (IR) or phase sensitive inversion recovery (PSIR) using ECG gated, spoiled gradient recalled echo (SPGR) or single shot steady state free precession (SSFP).
- The inversion recovery time is typically chosen to null the normal myocardium 6–15 minutes following administration of gadolinium.
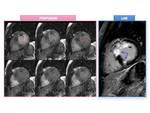
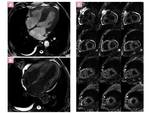
- Hyperenhancement of hypertrophic myocardium is frequently seen in as many as 80% of the patients with HCM Fig. 5
-Is the most valuable MR imaging sequence for HCM, identifies myocardial fibrosis or scarring that contributes to risk stratification. It is significantly related to ventricular tachyarrhythmia and SCD associated with HCM
- LGE of ≥15% of an LV mass was associated with a 2-fold increase in SCD event risk (Maron et al) Fig. 8
-LGE patterns reflects different types of HCM fibrosis:
- Replacement fibrosis: The magnitude of replacement fibrosis is variable and correlates with severity of LV remodeling and dysfunction.
-
-
Seen in the midwall (mesocardium) of the most hypertrophied segments.
-
Typical midwall patchy or confluent intense LGE Fig. 5
-
Transmural fibrotic tissue gives rise to pseudo-infarct patterns Fig. 8Fig. 9
-
End-stage transmural enhancement
-
Transmural fibrosis in apical aneurysms
-
Fibrosis due to increased extracellular matrix commonly seen at the junction of the right ventricle with the LV—likely due to a different, nonischemic mechanism.
-
Fine interstitial Fibrosis that is diffusely found in HCM midwall.
-
In our experience probably reflected by the light diffuse and confluent pattern of midwall LGE. Fig. 6 Fig. 7
-
The stimulus for interstitial fibrosis, reflecting exaggerated activation of the matrix, may be present before the development of cardiac hypertrophy in genotype-positive individuals.
-
Conspicuity in LGE patterns makes difficult the analysis for quantification of LGE. Harrigan et al showed that use of 6 or more standard deviations from normal myocardial intensity had the best correlation with visual assessment. However, validation data myectomy specimens from HCM patients showed 5 standard deviations to have the strongest correlation with total (ie, combined interstitial and replacement) fibrosis, whereas the best correlation with replacement fibrosis was obtained at 10 standard deviations. Fig. 7
-
Diferential diagnosis from Phenocopies with different pattern of fibrosis.
-
Evaluation of effects of therapy (scar tissue)
-
Identificate thrombus formation in left atrial appendage (atrial fibrillation)
-PERFUSION IMAGING
T1-weighted multi-slice gradient echo 1st pass gadolinium perfusion
-Provides information about blood flow and myocardial circulation with high spatial and temporal resolution. Allows evaluation of Microvascular function by identification of perfusion defects:
- microvascular obstruction with infarct-like pattern usually in areas of more hypertrophied and fibrotic myocardium. Fig. 9Fig. 9
- Perfusion tecniques are more sensitivy than LGE for detecting microvascular obstruction
-Usually performed at rest in patients with HCM because the stress test can provoke a LVOT obstruction or sudden changes in blood pressure, which can lead to serious symptoms.
-Several studies show the close relationship between perfusion decrease and wall thickness, LGE, or hyperintensity on T2-weighted images, suggesting that microvascular abnormalities precede and predispose to development of myocardial fibrosis ; thus, these perfusion abnormalities may represent an early risk marker (Noureldin et al). However the advantage of perfusion MR imaging over LGE and T2-weighted imaging have not been validated in HCM
-T2-WEIGHTED IMAGING/T2 MAPPING
-T2-weighted imaging in combination with double inversion recovery black blood preparation shows myocardial edema or inflammation associated with HCM, which may be related to chest pain, syncope, or increase in troponin.
- Myocardial hyperintensity on the T2-weighted image reveals myocardial edema (eg, acute ischemia) Fig. 10
- Myocardial severe fibrosis or collagen deposition shows signal hypointensity Fig. 10
-T2 mapping is useful for confirming the presence of myocardial hyperintensity on T2-weighted images (edema).
TAGGING MRI
-Myocardial deformation analysis
-Evaluating the myocardial wall motion and strain quantitatively. Show regional strain abnormalities even in the non-hypertrophied myocardium. Is a reproducible tool for multidimensional strain quantification.
-The hypertrophied myocardium with LGE tends to show decreased wall motion on tagging.
T1 MAPPING MRI (MOLLI, ShMOLLI and SASHA) Fig. 10 Fig. 11 Fig. 11
-Usually performed before (Native T1) and 15 min after the administration of gadolinium-based contrast agent.
-Tissues with an expanded extracellular space due to fibrosis, infiltration or scarring have a larger distribution volume for the extracellular contrast agent, and consequently the reduction in T1 relaxation time is more pronounced than in normal tissue. From pre- and post-contrast T1 maps, the extracellular volume (ECV) fraction may be calculated as:
»ECV = (1 – Hct) R1 (myo pre contrast) - R1 (myo post contrast)
R1(blood pre contrast) - R1( blood post contrast)
- T1 mapping MR imaging techniques are able to identify myocardial injuries associated with HCM without gadolinium-based contrast agents (Native T1 values).
-
Native T1 values and ECV are elevated in HCM and lower post-contrast T1 value (Ying Liu et al). The native T1 values of the myocardium are increased not only in the regions showing LGE but also in those without LGE in HCM. ECV is highest in regions with replacement fibrosis detected on LGE imaging.
-
Post-contrast myocardial T1 has been shown to significantly correlate with histological areas of fibrosis.
-
Native T1 value and ECV also appear to be elevated in regions without overt LGE suggesting that they are able to detect more diffuse fibrosis not seen on LGE imaging.
-
ECV fraction differs between HCM and Phenocopies ( Swoboda et al) and is positively correlated with the maximum wall thickness in HCM.
-
ECV is also increasd in mutation carriers without LV hypertrophy, Fibrotic remodeling is an early feature in the pathogenesis of the disease, (Ho et al )
-
T1 measurements correlated well with markers of collagen synthesis, suggesting that this technique may help monitor disease progression as well as to evaluate novel disease modifying therapy, targeting interstitial fibrosis.
RESEARCH TECHNIQUES:
-Diffusion imaging
- The hypertrophied areas also show significant reduction of diffusion anisotropy at diffusion-weighted imaging due to an increase in the longitudinally oriented fibers
- Myofiber disarray may be represented with DTI image
-MR spectroscopy
- The phosphocreatine (PCr)/adenosine triphosphate (ATP) ratio measured at cardiac MR spectroscopy is significantly reduced in hypertrophied myocardium in HCM patients compared with that in control subjects (Noureldin et al)
We resume and summarize in table -1 Fig. 12 MRI study protocol for HCM
2-CARDIAC MRI FINDINGS OF HCM
-PHENOTYPES OF HCM:
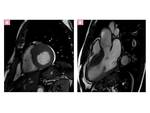
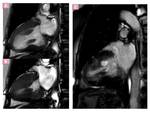
-Diagnostic criterion for HCM is a maximal LV wall thickness ≥ 15 mm in the end-diastolic phase. Fig. 1
-The morphologic expression of HCM is widely variable and heterogeneous because HCM may affect any portion of the left ventricle.
- In most HCM patients the hypertrophied myocardium follows a longitudinal pattern along a spiral trajectory in a counter clockwise direction from the base to the apex of the LV. The magnitude of spiraling ranged from minimal—following an almost straight trajectory—to marked, covering nearly the entire circumference of the LV. Fig. 13
- ASYMMETRIC (SEPTAL) HCM Fig. 14
-APICAL HCM (APH)
Predominantly involves the apical myocardium. It is also known as Yamaguchi syndrome and is characterized by the presence of giant negative T waves on the electrocardiogram. Major incidence in the Japanese population.
- Cardiac MR imaging identifies this phenotype of HCM more commonly than does echocardiography because of its no limited view.
- Absolute apical wall thickness > 15 mm or a ratio of apical to basal LV wall thicknesses of 1.3–1.5
- Characteristic “spadelike” configuration of the LV cavity at end diastole Fig. 17
- Predilection for middle-aged men
- Rarely associated with sudden cardiac death, has a relatively good prognosis. However, one-third of patients with APH present with ventricular tachyarrhythmia and have a worse outcome.
- Extensive LGE is related to ventricular tachyarrhythmia even in cases of APH Fig. 18
-MASS-LIKE HCM
Manifests as a masslike hypertrophy because of the focal segmental location of the myocardial disarray and fibrosis which may be differentiated from neoplastic masses. MR imaging with spin-echo pulse sequences, first-pass perfusion, and the DE technique helps to differentiate between the two entities.
-
Masslike HCM usually shows the homogeneous signal intensity characteristics and perfusion of adjacent normal myocardium, and typical patterns of LGE Fig. 19 , whereas tumors show heterogeneous signal intensity and enhancement and show perfusion characteristics that differ from those of the remainder of the left ventricle Fig. 20
-
Myocardial tagging with the steady-state free precession technique is also useful in differentiating the masslike HCM from a tumor because of the absence of active contraction in tumors, in comparison with the presence of contractility in HCM.
-SYMMETRIC HCM(Concentric HCM)
Is the second most common phenotype and is characterized by diffuse concentric thickening of the LV with an associated decrease in the size of the LV cavity and no evidence of a secondary cause. Fig. 6 y Fig. 21
-
Symmetric HCM is known to occur in as many as 42% of the cases of HCM.
-
Cardiac MR imaging plays an important role in differentiating other causes of symmetric myocardial hypertrophy: athlete’s heart, amyloidosis, sarcoidosis, Fabry disease, hypertension or aortic stenosis (see below in section phenocopies )
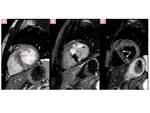
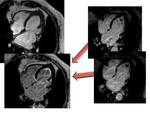
-MIDVENTRICULAR HCM Fig. 22
Is a rare variant of asymmetric HCM characterized by Hypertrophy occurring predominantly in the middle third of the LV wall and by systolic apposition of the mid-ventricular wall causing Midventricular obstruction (MVO). May be associated with an apical aneurysm caused by increased systolic pressures in the apex from midventricular obstruction. The importance of this variant is its association with ventricular arrhythmia, myocardial necrosis, and systemic embolism.
MR imaging shows:
-
“Dumbbell” configuration of the LV cavity with marked muscular midcavity systolic constriction
-
Cine SSFP identifies the jet flow and midventricular hypertrophy in MVO.
-
Cine SSFP images show apical aneurysm and LGE MR imaging shows where an apical aneurysm Fig. 23 has been replaced by scar tissues and also delineates apical thrombus which are significantly related to adverse cardiac events.
-RIGHT VENTRICLE (RV) INVOLVEMENT
Is seen in up to 17% of cases with HCM. The RV is involved as a consequence of direct injury extension and afterload changes.
-
RV involvement, predominantly affects the mid to apical portion Fig. 24
-
CMRI is the most valuable imaging technique to delianete RV hypertrophy because echocardiography is limited for RV evaluation
-
Although a right ventricular outflow obstruction may occur in association with right ventricular myocardial hypertrophy, its clinical significance remains unknown in HCM.
-PAPILLARY MUSCLES ANOMALIES, MUSCLE BUNDLES AND CRYPTS
1-Papillary muscular abnormality are often investigated in patients with HCM and include:
-
hypertrophied papillary muscles, increase in the number of muscles Fig. 25, and abnormal attachment of the muscles to the mitral valves or interventricular septum, apical implantation often investigated in patients with HCM.
-
Anteroapical displacement of the anterolateral papillary muscle may contribute to the severity of LV outflow obstruction
-
LGE may be observed in hypertrophied papillary muscles Fig. 22 .
-
Isolated PM hypertrophy is a possible variant of HC (Correia et al)
-
Solitary papillary muscle hypertrophy can produce left ventricular mid-cavity obstruction thus carries clinical importance, (Kuo-Tzu Sung et al)
2-Apical –basal muscle bundles are a unique myocardial structure commonly present in HCM patients as well as in G+/P2 family members and may represent an additional morphologic marker for HCM diagnosis in genotype-positive status. Fig. 26
3-Myocardial crypts are narrow, deep invaginations within the myocardium localized predominantly in the basal posterior septum and LV-free wall. They are congenital fissures related to the disarray of the myocardial fibers. Fig. 26
-
CMR has enabled in vivo detection of crypts: Fig. 27 as discrete approximately V- or U-shaped extension of blood signal, on cine viewing to penetrate more than 50% of the thickness of the adjoining compact myocardium in diastole” narrowing or completely occluding in systole, without segmental contractility defects.
-
Is considered one of the morphological signs of genotype positive/phenotype negative subjects. Germans et al. found crypts in 81% carriers of HCM mutations. In contrast, Petryka et al. reported a prevalence of 15.6% in HCM, 13.6% of hypertensive patients and 6% of healthy volunteers.
-
Crypts may be significant findings in a familial context with a high probability of HCM, their clinical significance is doubtful as isolated findings in asymptomatic patients, probably representing, in these cases, only incidental variants.
3-CLINICAL MANIFESTATIONS, COMPLICATIONS, AND NATURAL HISTORY
Phenotypic expression of HCM with LV hypertrophy generally occurs in adolescents. An early-onset form occurring in infancy and early childhood and a late-onset form occurring in midlife exist.
There is an increasing population of asymptomatic genotype-positive but phenotype-negative family members, in whom long-term monitoring with CMRI is very relevant
It is important to make a distinction between phenotype-negative HCM and “NON-HYPERTROPHIC” HCM, displaying:
In most patients, a lifelong process of progressive cardiac remodeling with increasing myocardial fibrosis takes place. Cardiac remodeling with overt NYHA class III - IV heart failure occurs in a 2%–5% of patients (obstructive phenotype or restrictive phenotype)
-DIASTOLIC DYSFUNCTION AND PULMONARY HYPERTENSION
Diastolic abnormalities are highly present and can be detected in genotype-positive individuals before significant hypertrophy or clinical symptoms appear. Impaired LV diastolic function is a major pathophysiologic feature in all patients with HCM.
-
Cardiac MR imaging is increasingly being used to assess diastolic function by means of velocity encoding and spatial modulation of magnetization(SPAMM) sequences .
-
Independent of hypertension or the presence of coronary artery disease Left ventricular hypertrophy is the most common structural abnormality in patients with with heart failure with preserved ejection fraction (Webb et al).
Pulmonary hypertension is common in obstructive HCM patients with severe heart failurean but there is no agrrement about if it is marker for identification of those patients who may benefit from surgical abolition of the outflow gradient or not.
CMR allows accurate assessment of the right ventricle function and volumes, pulmonary artery flow and diameters.
-SYSTOLIC DYSFUNCTION, END-STAGE HCM
HCM usually shows normal or supernormal systolic function of the left ventricle, ejection fraction up to > 75%. However, approximately 15% of patients with HCM show LV ejection fraction (LVEF) between 50%–65% indicating adverse remodelling and 5‒10% of patients show LVEF< 50%, which is called “end-stage” or “burn-out” HCM. Indicates a poor prognosis in the 5 years at its initial diagnosis because of heart failure and thromboembolic complications but also from a substantial incidence of SCD.
Cardiac MR imaging is able to measure the ejection fraction accurately and demenstrate de differnt patterns of systolic dysfunction:
4-CLINICAL RELEVANCE OF CMRI TO HCM
-DIFERENTIAL DIAGNOSIS - PHENOCOPIES
HCM phenocopies is refered to several genetic conditions that are not caused by cardiac sarcomere mutations, associated with severe LVH. include a variety of disorders such as glycogen storage disorders, lysosomal storage disorders (Anderson-Fabry Disease Fig. 28Fig. 32 ), mitochondrial cytopathies, cardiac amyloidosis Fig. 31 and disorders of fatty acid metabolism. LVH is also observed in, hypertensive cardiomyopathy, and aortic valvular disease and Athlete’s heart. Athlete’s LVH should be differentiated from HCM, because SCD can occur in young athletes with HCM.
Cardiac MR imaging is valuable for differentiating between HCM and other myocardial diseases showing LVH Fig. 29 because of its accurate identification of:
-
The patterns of myocardial hypertrophy and LGE.
-
basal crypt, accessory apical-basal muscle bundle and apical pouching which can suggeste the diagnosis of HCM
-
T1 native and postcontrast ECV values elevated in HCM Fig. 30
Other more rare phenocopies include:
-
Endomyocardial fibrosis Fig. 33 (Löffler endocarditis and endomyocardial disease) is a rare form of restrictive cardiomyopathy.MR imaging is particularly helpful in differentiating this entity from apical HCM, allowing evaluation of the fibrous endocardial thickening and LGE in fibrotic áreas, myocardial inflammation, apical or subvalvular obliteration, thrombus formation, and restrictive LV physiology.
-
LV noncompaction (LVNC): isolated noncompaction may mimic apical HCM at echocardiography when particularly severe and occurring at midapical LV. MRI allows differentiate excessively prominent trabecular meshwork and deep intertrabecular recesses of LVNC form compacted myocardial thickening of HCM.
-
Primary and secondary cardiac tumors. Fig. 20
4-RISK STRATIFICATION
The risk stratification for HCM, especially the risks for SCD, is generally assessed based on the clinical and family history, patient’s age, and electrocardiogram findings.
|
Major risk markers and risk modifiers associated with increased risk of sudden cardiac death (SCD) in hypertrophic cardiomyopathy
|
|
Major risk factors
|
|
Family history of sudden cardiac death
|
|
Nonsustained ventricular tachycardia
|
|
Syncope
|
|
Maximal left ventricular wall thickness
|
|
LV apical aneurysm
|
|
End-stage HCM
(LVEF
|
|
Risk Modifiers
|
|
Marked LV outflow tract obstruction
|
|
Late gadolinium enhancement by CMR
|
|
Age
|
|
Abnormal blood pressure response to exercise
|
Cardiac MR imaging is valuable because of its ability to depict accuretly:
-
Left Ventrice ejection fraction( LVEF<50% is a major risk factor)
-
Myocardial thickness and myocardial mass accurately. Massive hypertrophy and maximum wall thickness (wall thicness>30mm Fig. 34 , major risk factor os SCD)
-
Identify myocardial fibrosis noninvasively and cuantify LGE enhanacement porcentage (risk modifier). LGE reflects replacement and interstitial myocardial fibrosis and associated coronary artery dysplasia. Extensive LGE can indicate risks for the ventricular tachyarrhythmia or systolic impairment associated with HCM.
-
LGE of ≥15% Fig. 35 of an LV mass was associated with a 2-fold increase in SCD event risk. the extent of LGE is strongly associated with the risk of SCD, thus, the extent of LGE may be a more potent marker than its presence alone (Kramer et al)
-
Maron et al:"LGE represents a novel powerful clinical tool that dictates HCM clinical course along 2 divergent adverse pathways: risk for sudden death and for advanced end-stage heart failure. For these and other reasons, it would seem justified to regard CMR as firmly integrated in the contemporary assessment of virtually all HCM patients".
-
Evaluate risk phenotypes:
-
Midventricular obstruction, that is is a “high-risk” type of HCM, especially when it is associated with apical aneurysm, possibly leading to ventricular tachyarrhythmia or systemic thrombosis.
-
advanced fibrotic remodeling of the LV, such as apical aneurysms and end-stage HCM, LVEF<50%, both identify subsets with markedly increased risk of SCD, warranting aggressive management.
- LV outflow tract obstruction: basal gradient ≥ 30 mm Hg or of ≥50 mm Hg with exercise, (risk modifier)