PROCEDURE DETAILS
We interrogated our institution’s Radiology Information System (RIS) for MRI brains performed under general anaesthesia within 14 days of suspected global ischaemic insult over a 9-year period.
472 scans were performed within this time period under those conditions. All scan reports were analysed by the lead author and were included in the study if the initial report was positive for anoxic brain injury. Demographics and clinical outcome measures were recorded by the lead author. Clinical outcome was adjudicated by calculating modified rankin score (mRS) at the time of discharge based on a retrospective electronic chart review [2].
A retrospective analysis of T2W/FLAIR, B1000 images and ADC maps was performed to determine the distribution, extent and combination of findings. Images were reviewed for grey matter hyperintensity and graded as diffuse if more than 70% of the cortex was involved or patchy if less than 70% involvement. To replicate clinical reporting this was performed based on visual estimation by an experienced consultant neuroradiologist. Deep nuclei, brainstem and cerebellar involvement was also evaluated.
Qualitative analysis was performed on all cases comparing TSE-T2 with FLAIR and FLAIR with DWI B1000. We evaluated pathology conspicuity on a particular sequence to ascertain superiority or equivalence between the two sequences. We subdivided our analysis of DWI and FLAIR between those patients imaged between 1-5 days and 6-14 days. We also performed a qualitative analysis of the concordance between a patients DWI and ADC images- where high signal was observed on DWIB1000 images, was there corresponding low signal on the ADC map and vice versa.
Statistical analysis was performed using Chi Square for categorical variables and students t test with a two tailed hypothesis for continuous variables. Results were considered significant where p<0.05.
FINDINGS
We identified 71 patients with diffuse anoxic brain injury over the 9 year period (mean age 57 years, range 23-83yrs) (M:F 49 (69%):22 (31%)). The average time from cardiac arrest to MRI was 5.03 days (range 1-13d). 31% of cases were due to acute coronary events, 8% to drug overdoses, 10% to asphyxia, 32% to miscellaneous causes including perioperative and in 18% the cause of the event was not identifiable.
Imaging Patterns
There was considerable overlap between all the patterns observed. The most common imaging pattern observed was bilateral thickening and hyperintensity of the cortical ribbon occurring in 92% of cases (Total n=64; diffuse n=50, patchy n=14). N=65 (92%) of cases demonstrated some form of deep gray matter nuclei involvement with the caudate (n=65) and putamen (n=63) nuclei most frequently affected. 10% (n=7) demonstrated extensive white matter infarction with both diffuse and patchy grey matter involvement associated. A watershed cortical pattern was observed in 2 cases. No cortical involvement was identified in n=2 cases.
MRI Sequences
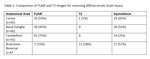
Comparing Diffusion-Weighted imaging and FLAIR sequences (table 1) for evaluating the cerebral cortex, where imaging was performed within 5 days of the ischaemic insult, we noted 57% (n=25) of cases were visualised better with DWI while just 2% (n=1) had increased lesion conspicuity on FLAIR. Equivalence between the two techniques was found in the remaining 41% (n=18). In contrast; when performed outside that initial 5 day window 32% (n=7) were visualised better with B1000, 27% (n=6) with FLAIR and in 41% (n=9) there was no difference found between the two sequences.
In assessing lesion conspicuity on FLAIR and TSE T2 (table 3), FLAIR imaging was consistently superior (54%; n=35) or equivalent (45%; n=29) to TSE T2 for assessment of the cerebral cortex. For the basal ganglia, in 46% (n=31) cases FLAIR was superior to T2 while in the remaining 54% (n=36) there was equivalence between the two methods. On review of the cerebellum, lesions were more conspicuous on FLAIR in 75% (n=41) and equivalence was achieved in 25% (n=14). The brainstem reversal sign was more prominent on FLAIR in 15% (n= 7), TSE-T2 in 27% (13) and equivalent in 56% (n= 27) of cases.
38 patients (out of n=66 patients with cortical involvement; n=44 imaged <= 5 days; n=22 imaged > 5 days) had ADC maps which were concordant for the cerebral cortex with their associated B1000 diffusion imaging. Of these 38, 82% (n=31) had their imaging performed within 5 days, 18% (n=7) had imaging performed outside the 5 day window. This was a significant difference (p value 0.0028 by Chi Square). 6 patients (9%) had ADC-DWI concordance for basal ganglia lesions while just 3 patients (5%) had cerebellar concordance. All cases of concordance for the basal ganglia and cerebellum occurred on imaging performed between 1 and 5 days post injury. There were 7 cases involving significant white matter anoxic injury; n=6 of these had concordant ADC/DWI imaging.
Outcomes
Survival to tertiary hospital discharge occurred in just 24% (n=17) of cases, n=6 of these survivors had severe disability with a mRS of 5. Within the diffuse cortical infarction category n=46 (92%) had an mRS of 4-6 at the time of discharge. 11 cases (79%) of patients with patchy cortical infarction had an mRS of 4-6 at the time of discharge which was non-significant compared to those with diffuse cortical involvement (chi square 2.02; p=0.15). All patterns were associated with a poor clinical outcome (mRS 4-6). No specific pattern was significantly associated with a good clinical outcome.