Type:
Educational Exhibit
Keywords:
Abdomen, Gastrointestinal tract, Paediatric, CT, Nuclear medicine conventional, Ultrasound, Surgery, Congenital, Diverticula
Authors:
A. Lopez Maseda, I. Moreno Ochoa, A. Garmendia Zabaleta, E. García Serrano Fuertes, C. Galvez Estevez, A. Gozalo García, S. Larburu Zavala, J. M. Pérez Roldán, I. Arteche Arnaiz
DOI:
10.26044/ecr2022/C-12856
Findings and procedure details
The main complications of the Meckel diverticulum are as follows:
- Gastrointestinal bleeding: is the most common complication, accounting for around 30% of symptomatic Meckel diverticula. Usually occurs associated to the presence of ectopic gastric mucosa. It normally consists of a self-limited bright red rectal bleeding, though sometimes can be life threatening [2-6,8-10]. Imaging features include:
- 99mTc-gammagraphy: useful in the detection of ectopic gastric mucosa in a suspected Meckel diverticulum. It may show radiotracer uptaking focus in the lower abdominal region, most frequently in the right lower quadrant. A normal scintigraphy does not rule out Meckel diverticulum as the source of the gastrointestinal bleeding, presenting a false negative rate between 20-35% [3,7](Fig. 18).
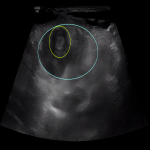
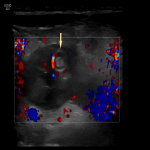
- US: might show the ultrasonographic features of the uncomplicated Meckel diverticulum, as the ectopic mucosa does not have any sonographic distinctive feature (Fig. 15-17).
- Angiography: can show active contrast extravasation arising from superior mesenteric artery branches (onphalomesenteric arteries) in the setting of severe gastrointestinal bleeding (more than 0,5 ml/min) [6]. In cases of active extravasation, angiography might not only be diagnostic, but also serve as a therapeutic tool.
- Obstruction: the second most common symptomatic presentation (some published studies even refer to it as the most common) [3,6,8-10]. It can be secondary to mesodiverticular bands, Meckel intususception or Littre's hernia (hernia containing Meckel diverticulum, frequently inguinoscrotal). The larger the diverticulum, the greatest the risk for intestinal obstruction.
- Plain film: nonspecific, demonstrating small bowel loop dilatation with or without colon distention (Fig. 21).
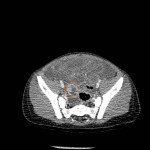
- Abdominal CT scan: helpful in the depiction of the abrupt intestinal caliber change indicative of bowel obstruction, though it might not reflect the exact cause (Fig. 26).
- Intususception: a "bowel-within-bowel sign" can be seen with an intraluminal mass within the dilated outer intestinal loop (intususcipiens) [11].
- Littre's hernia: typical CT features are the presence of a tubular blind-ending structure arising from the small bowel in a hernia + intestinal obstruction.
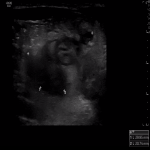
- Ultrasound: usually performed in the setting of intestinal obstruction in children, will show dilated bowel loops and may show features of intususception and/or complicated herniae (Fig. 7, 22).
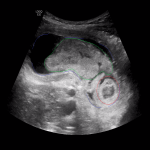
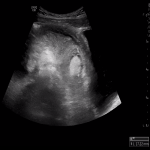
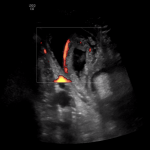
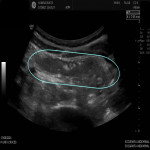
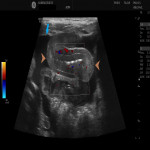
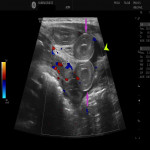
- Intususception: better depicts the "target sign", with the invaginated bowel loop (intususceptum) and an accesory tubular structure (the Meckel diverticulum that serves as the leading point) inside the intususcipiens [11] (Fig. 1-2, 6). Meckel diverticulum related intususceptions are most frequently ileo-ileal due to the anatomical disposition [3,8-10] (Fig. 1-5), but can eventually progress and become ileo-cecal (Fig. 6). In the latter case, cecal appendix may be also identified within the intususcipiens and serve as a pitfall.
- Littre's hernia: a tubular blind ending structure arising from the small bowel within a inguinal hernia + small bowel dilatation.
- Diverticulitis: Meckel diverticulum inflammation accounts for up to 19% of complications. Both obstruction and diverticulitis are the most common complications in adult population [5]. It may be secondary to chemical acid secretion irritative effect of the ectopic gastric mucosa or obstructive due to enterolith formation [3,6].
- Abdominal CT: may depict hyperenhancement and peridiverticular fat stranding as inflammatory imaging markers, similar to the findings of acute appendicitis or acute bowel diverticulitis [9,10,12,13].
- US: ultrasonographic findings of Meckel diverticulitis consist on enlargement, noncompressibility of the diverticulum and peridiverticular fat hyperechogenicity (Fig. 28-30). Intraperitoneal free fluid might appear in cases of severe inflammation. Doppler ultrasound may show hypervascularization of the swollen loops and the adjacent fat [9,10,13].
- Perforation: it is a rare and severe complication, even though some publications have described it in up to 11% of complicated Meckel diverticula. It might be secondary to Meckel diverticulitis (Fig 28-30) or peptic ulceration in the presence of ectopic mucosa [3, 6, 8-10]. Imaging findings suggestive of perforation are pneumoperitoneum and/or intraabdominal free fluid.
- Neoplasm: a late complication, it has been described in 1-3% of patients with Meckel diverticulum, most frequently presenting in adult patients. Carcinoid tumor is the most common tumor, theoretically arising from ectopic gastric or pancreatic mucosa. Other histologic subtypes include lipoma, leiomyoma, mucocele and adenocarcinoma, to name a few of them [3,6]. No distinctive imaging findings have been described for the former neoplastic subtypes in Meckel diverticula.
- Other complications: such as chronic relapsing pain episodes, abscesification of other remnants of the persisten onphalomesenteric duct,... [6] are very unfrequent and beyond the scope of this text.
We present a series of cases depicting some of the aformentioned complications:
- Case nº1: ileo-ileal intestinal intususception secondary to a Meckel diverticulum (Fig. 1-5).
- Case nº2: ileo-cecal intususception due to a Meckel diverticulum (Fig. 6)
- Case nº3: Meckel diverticulum torsion and intestinal obstruction caused by a mesodiverticular band (Fig. 7-14).
- Case nº4: Rectal bleeding caused by a Meckel diverticulum (Fig. 15-20).
- Case nº5: Meckel diverticulitis causing secondary obstruction (Fig. 21-27).
- Case nº6: Perforated Meckel diverticulitis (Fig. 28-30).
Some of the explained complications may coexist and appear simultaneously, as can be seen in cases nº3, nº5 and nº6.