Congress:
EuroSafe Imaging 2020
Keywords:
Multicentre study, Observational, Retrospective, Quality assurance, Education and training, Safety, Health policy and practice, Dosimetry, CT, Radioprotection / Radiation dose, Radiographers, Action 5 - Performance indicators for radiation protection management
Authors:
T. Szczykutowicz, S. Rose
DOI:
10.26044/esi2020/ESI-02989
Conclusion and recommendations
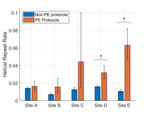
Figures 4 and 5 depict the results of applying a repeat rate analysis to two different imaging centers. Figure 4 quantifies the repeat rates while Figure 5 quantifies effective dose differences for exams with and without a tomographic (i.e. axial or helical scan) repeat.
- Repeat rates at the sites we studied are much lower than those reported for radiography and mammography[3]
- Effective dose increases are actually more than double for exams containing repeats. We believe they average over 100% increase because larger patients tended to be more likely to have a repeat relative to smaller patients--> driving the effective dose for repeat containing exams up.
What to do with all this data?
- Now we can identify areas for targeted improvements efforts. We can quantify repeats by scan type and specific: sites, scanners, protocols, technologists
- Technologists with 0% repeats likely are NOT doing a good job. Some repeats are motivated by patient motion or poor patient cardiac output. A good technologist would repeat an exam to account for these clinical realities.
- Technologists with high repeat rates relative to their peers may not be giving adequate patient instructions, or interacting with the CT scanner properly.
- Protocols with high repeat rates may signal issues with the scan parameters. For example, high rate of repeats for a specific pediatric protocol due to motion may motivate speeding up the protocol.
An example of what a site can do once they have repeat rate analysis data. We applied our repeat rate data to 5 unaffiliated sites. We quantified the repeat rates for CTA for PE across the sites and found a statistically significant difference between sites. See Figure 6. Further analysis of the difference between sites discovered the sites with higher CTA for PE repeats were using: higher gauge needles for contrast administration, had more frequent injector malfunctions, and did not use a contrast warmer. All of these difference help explain why their high injection rate CTA for PE exams were being repeated due to poor contrast enhancement.
Conclusions
- We have provided an overview of the causes, effects, and impacts of repeated imaging in CT.
- We have defined distinct types of repeats for CT representing scan modes: localizers, bolus tracking, helical, axial, and extension repeats
- We have quantified repeat rates for the first time, reporting tomographic (i.e. helical and axial) rates were 1.2% from a cohort of 61,102 patients
- We have quantified for the first time effective dose increases due to repeated imaging
- We have shown an example of how repeat rate analysis can be used to direct a quality/safety teams efforts
- We need to apply our methods to sites that do not cultivate their protocols like we do. We know from the literature, repeat rates are effected by the work of a CT protocol optimization team.[5] Our main site has direct oversight by such a team[6-7], and we advise the rural site included in our study.