Interventions made to lower the doses and reduce the number of unnecessary paediatric CT investigations:
Awareness and education:
- Discussions in the radiology department, educational lectures in the radiology department for radiographers and radiologists.
- Educational lectures in different referring departments.
- Educational lectures at the national meetings of different organizations (Estonian Society of Radiology, Estonian Society of Radiographers).
- Refresher courses for physicians and radiographers.
- Lectures for medical students and residents about the optimal use of CT for children.
Technological updates:
- The older CT machines were replaced by up-to-date machines by the beginning of the year 2017.
- All investigations in children were encouraged to be performed only with the newest scanner with known lower doses in all body regions.
- CT protocols for paediatric patients were reviewed by physicists and changed if needed to reduce dose.
- For all children, appropriate paediatric protocols must be used.
Organizational updates:
- Emergency paediatric CT investigations - referring physician discusses the case with the radiologist to ensure that CT is the optimal investigation.
- Radiographers do not start any paediatric study without the permission of the radiologist.
- Electronically scheduled outpatients - radiologist reviews referral request and if needed suggests MRI examination.
- Radiologist is present in the examination suite during paediatric CT investigations and makes the choice of the protocol: usually only one phase is needed.
Study materials and methods:
In the year 2017 (31.01.2017- 31.01.2018) data about all CT studies in children aged 0-16 performed in our institution were prospectively collected. Similar study performed in the year 2012 (1.11.2011 -10.08.2012) was used for comparison.
Patients age, weight, height and referral diagnosis for the examination were recorded on a special survey form. CT dose index (CTDIvol), dose-length product (DLP) and phantom diameter used for calculations were collected from dose protocols from Estonian PACS (Picture Archiving and Communication System) using special referral numbers. Patients were divided into four age-groups (<1y, 1-4y, 5-9y, 10-16y) and the CT studies were grouped by the body parts examined and the clinical indications of the studies.
Local DRL (Dose Reference Levels) were calculated for both years using the 75th-percentile value of the distribution of patient doses in CTDIvol and DLP, providing the age group contained the dose data from at least ten patients. In our small cohort, only examinations of the head had enough patients in most of the age groups. In addition, only head studies with the standard protocol were used for calculations of LDRLs. Results were compared to international DRL values from Vassileva et al [2].
Statistical data from Estonian PACS was used to evaluate the trends in the usage of paediatric CT and MRI in our institution.
Results:
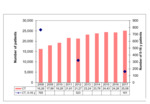
The overall number of CT investigations in Tartu University Hospital has increased yearly, from 16260 examinations in 2008 to 25085 examinations in 2017. During the last 10 years, the number of patients in CT has increased by 54% in our hospital ( Fig. 1 ).
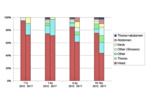
By the year 2017, the number of CT investigations in children in our institution had decreased 4,75 times compared to the year 2008. During the study period of 2017, the number of paediatric CT examinations was two times lower (p<0.0001, OR=2.6 95% CI: 2.2-3.2) than in 2012. In 2012 31% of paediatric investigations were done in CT and rest in MRI, in 2017 only 24% were done in CT and rest in MRI.
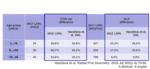
The rate of head CT examinations decreased from 87.8% to 63.8% (p<0.0001, OR=4.1 95% CI: 2.6-6.4) of all CT investigations in children. The number of paediatric CT investigations of chest and abdomen had no significant difference during the years (Fig. 2). The indications for paediatric head CT stayed mostly the same, but the rate of CT examinations for headache reduced significantly (Table 1).
Only one body region was investigated in 86% of patients in 2012 and in 89% of patients in 2017. Usually, one phase scan was used, but contrast enhancement was used in 8% of examinations in 2012 and 9.3% of examinations in 2017 (p=0.8).
79 examinations of the head were applicable for the calculations of LDRLs in 2017 and 215 examinations in 2012. Head CT LDRLs were lower in 2017 compared to 2012 in all age groups, by 28,6-66,7%(CTDIvol16) or 5,2-23,3% (DLP16). Compared to international data LDRLs were lower by 30,6-15,1% (CTDIvol16) or 20,9-5% (DLP16) ( Table 2 ).