Congress:
EuroSafe Imaging 2020
Keywords:
Performed at one institution, Not applicable, Cancer, Radiation effects, MR, CT, Radioprotection / Radiation dose, Head and neck, Head and Neck
Authors:
R. T. Le, F. Behzadi, P. Fiester, J. Patel, R. Dagan, D. Rao
DOI:
10.26044/esi2020/ESI-08297
Background/introduction
Over 500,000 new cases of head and neck cancer are diagnosed globally each year. The incidence has continued to rise in the United States, Canada, Western Europe, and Scandinavia since the 1980s [1]. More than 90% of head and neck cancer is squamous cell carcinoma [1], which is amenable to a combination of surgery, intensity-modulated radiation therapy (IMRT), and/or chemotherapy.
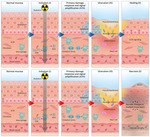
Mucosal cells experience high mitotic activity and are susceptible to the harmful effects of radiotherapy. Radiation exposure to the oral cavity and pharyngeal mucosa can lead to the development of radiation induced oral mucositis (RIOM). RIOM is a significant morbidity of radiotherapy, affecting over 80% of patients who require radiation for head and neck cancer management [2]. Sonis et al. [3] describes a five-phase cellular model for the development of RIOM [ Fig. 1].
-
Phase 1 (initiation phase): radiation creates double-stranded DNA breaks in cells, catalyzing endothelial damage
-
Phase 2 (epithelial phase): NF-kB and pro-inflammatory cytokine release, which may present as erythema
-
Phase 3 (cellular signaling and signal amplification phase): pro-inflammatory messengers (e.g. TNF-α) released, upregulating caspases and ceramide synthase, promoting cellular apoptosis
-
Phase 4 (ulceration): pro-inflammatory activities effects aggregate and develop mucosal breakage, resulting in fibrinous pseudomembrane formation -- a nidus for microflora or opportunistic infection
-
Phase 5 (healing): renewed epithelial proliferation and normal microbiome restoration, usually 3 weeks after radiotherapy or, if healing impaired, may progress to wound breakdown, ulceration, and/or permanent necrosis
Associated risk factors of mucositis include concurrent chemotherapy use, age greater than 65 years, poor oral hygiene, and co-morbidities including periodontal disease or diabetes [4]. Consequences of RIOM are the interruption of radiotherapy, which leads to poorer neoplastic control and compromises survival, and sub-optimal wound healing. Mucosal injury related to RIOM may follow different time courses between patients. Some patients may experience mild symptoms before complete healing, while others may experience more severe symptoms including mucosal ulceration and necrosis.
There is heterogeneity concerning timing and modality of post-radiotherapy imaging. Additionally, there may be wide variability between patient-reported symptoms, laryngoscopy imaging, and/or radiographic findings. As there are still knowledge gaps about this disease process, radiologists can fulfill an important role when encountering post-radiotherapy imaging by providing objective interpretations to subjective clinical complaints.