Learning objectives
To determine diagnostic accuracy of combined ultrasound and CT versus MRCP in evaluation of cause of obstructive jaundice patients presented to our Hospital
Background
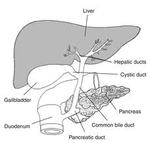
Disorders of the biliary tract affect a significant portion of the worldwide population,
and can pose problems in both diagnosis and management.Biliary obstruction refers to the blockage of any duct that carries bile from the liver to the gallbladder or from the gallbladder to the small intestine [Figure 1].
Cholestasis or failure of biliary flow may be due to biliary obstruction by mechanical means or by metabolic factors in the hepatic cells.Mechanical causes of biliary obstruction include intrahepatic and extrahepatic causes.Intracellular/ metabolic causes of cholestasis...
Findings and procedure details
We performed retrospective review of imaging in obstructive jaundice patients presented to our Hospital through out-patiet department (OPD) clinic and emergency,
in a period of 3 years (from September 2014 to September 2017).
This descriptive observational study was approved from Hospital Ethic & Research Committee.
All adult patients (aged more than 15 years) for whom ultrasound,
CT scan and MRCP performed,
were included.Patients' ages range between 26 to 85 years.Only patients with extra-hepatic mechanical causes of biliary obstruction were included.
Paediatric patients (of less than...
Conclusion
Ultrasound,
CT and MRCP are important diagnostic tools in evaluation of obstructive jaundice patients.
Each modlity has its own pros and cons,
and each alone may not be suitable or sufficient for all patients to reach diagnosis.
Despite its operator-dependent,
machine resolution-dependent,
technique-dependent factors,
and limitations because of patient habitus (obesity),
condition (old age,
poor breth-hold) and scanning (bowel gases),
ultrasound remains the first imaging modality of choice in obstructive jaundice patients as it is cheaper,
safe,
fast and readily available,
and can be performed...
Personal information
Dr.
Khawaja Bilal Waheed,
MBBS,
FCPS,
EDiR
Senior Specialist General Radiologist,Department of Radiology
King Fahad Military Medical Complex Dhahran,
31932,Saudi Arabia
Contact: 00 966 138440000 (Ext.
3222),
00 966 561299756
Email:
[email protected],
[email protected]
References
Singh A,
Mann HS,
Thukral CL,
Singh NR.
Diagnostic Accuracy of MRCP as compared to ultrasound/ CT in patients with obstructive jaundice.
J Clin Diagn Res.
2014 Mar; 8(3): 103-107.
10.7860/JCDR/2014/8149.4120
Petrescu I,
Bratu AM,
Petrescu S,
Cristian D,
Burcos T.
CT vs.
MRCP in choledocholithiasis jaundice.
J Med Life.
2015 Apr-Jun; 226-231.
Joshi A,
Rajpal K,
Kakadiya K,
Bansal A.
Role of CT and MRCP in Evaluation of Biliary Tract Obstruction.
Current Radiology Reports.
2014 Nov; 2:72.
Badger WR,
Borgert AJ,
Kallies KJ,
Kothari...