The study included 120 patients aged 65 to 90 years (average age 76.4±3.6 years) who were admitted for hospital treatment of different internal diseases.
Inclusion criteria: 1) the presence of at least 3 comorbid diseases of internal organs; 2) age over 65 years; 3) informed consent of the patient to participate in the study; 4) Clinical suspicion to any kind of lung pathology with indications to chest diagnostic imaging; 5) Availability of chest X-ray and chest CT performed during the hospital admission.
Exclusion criteria: 1) traumatic chest injuries; 2) pulmonary tuberculosis; 3) acute myocardial infarction 4) acute stroke
The study included patients with coronary heart disease (CHD), arterial hypertension (AH), chronic cardiac (CHF) and respiratory failure (RF), acute pneumonia, COPD, tumors and metastases to the lungs, diabetes mellitus, chronic kidney disease (CKD) and idiopathic pulmonary fibrosis (ILF). The frequency of detection of these diseases in patients included in the study is shown in figure 1.
As a part of the clinical examination, the standard chest X-ray was done in all patients with a digital system. For further clarification of X-ray findings, a standard chest CT (32-row CT scanner) was done in all patients.
In the majority of patients chest CT provided more accurate and full diagnostic information about the characteristics of lung pathology.
For example, in 36 patients chest CT detected a typical pattern of polysegmental acute pneumonia, but the initial chest X-ray found the definitive signs of pneumonia only in 12 cases (33.3%) (figure 2). In 11 of 24 patients (45.8%), the limitations of chest X-ray in the diagnosis of pneumonia was associated with the presence of signs of severe venous congestion due to CHF and in 6 of 24 patients (25.0%) due to signs of chronic obstructive bronchitis and diffuse pulmonary fibrosis.
X-ray signs of COPD and chronic obstructive bronchitis were detected only in 10 of 33 patients (30.4%) (in comparison with chest CT), bronchiectasis – in 2 of 8 (24.7%), signs of obturation and compression atelectasis – in 9 of 30 (30.0%), small post-inflammatory foci were detected in 13 of 56 patients (23.2%), areas of chronic pulmonary fibrosis in 14 of 38 patients (36.8%) and signs of hydrothorax - in 20 of 26 patients (76.9%) (figure 4).
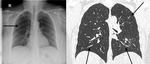
Chest X-ray detected central lung masses in 11 out of 12 patients (91.7%), while multiple peripheral lung metastases in oncological patients were detected only with the help of CT-study (figure 6).
The correct diagnosis of idiopathic pulmonary fibrosis according to the CT method was made in all patients, whereas in the study with the help of RG, the diagnosis was confirmed only in one of three patients (33.3%).
The reasons for the low efficiency of chest X-ray for early diagnosis of inflammatory lung diseases were: summation effect (42.1%), the presence of severe heart failure with signs of venous congestion in the lungs (45.8%), as well as incorrect interpretation of findings in radiographs (10.5%) (a subjective factor).