Keywords:
Oncology, Paediatric, Radioprotection / Radiation dose, MR, Radiation therapy / Oncology, Radiobiology, Biological effects, Cancer, Toxicity
Authors:
P. U. Sakhavalkar, S. Avula, N. Thorp, B. Pizer, M. Jenkinson
DOI:
10.26044/ecr2022/C-10308
Methods and materials
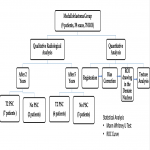
This is a retrospective review of 9 paediatric patients (a total of 39 scans) with medulloblastoma treated with surgery, photon radiotherapy and chemotherapy (Fig 1).
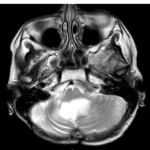
2-year and 5-year follow up T2 MRIs were qualitatively analysed by a paediatric neuroradiologist (SA) based on the presence or absence of progressive T2 hyperintensity in the cerebellum (Fig 2).
Patients were grouped according to the presence or absence of progressive T2 signal change (PSC) at 2-years and 5-years on qualitative analysis.
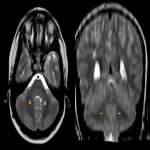
For quantitative analysis, all the follow up T2 scans were registered with the baseline scan of the individual patient and were bias-corrected. Regions of interest (ROIs) of 5mm were drawn at fixed locations (Fig 3) in the right and left visibly normal and homogenous cerebellar white matter in the dentate nucleus on all the T2 scans over 2-year period.
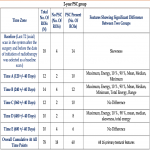
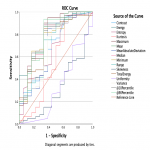
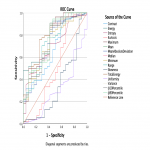
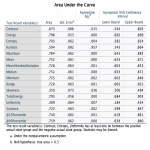
Areas with signal abnormality were avoided while placing ROIs. The radiation dose was calculated in these 78 ROIs and was found to be between 50-60 Gy. Texture analysis was performed. Sixteen primary textural features (contrast, energy, entropy, kurtosis, maximum, mean, mean absolute deviation, median, minimum, range, skewness, total energy, uniformity, variance, 10%, 90%) were extracted. Feature values between two groups were compared with Mann Whitney U test at different time points: Baseline, A, B, C, D, E and cumulatively at all time points together as described in Fig 5 and 6. Receiver Operator Characteristic Curve (ROC) analysis was carried out to determine the diagnostic performance of the radiomic features to distinguish between patients with PSC at 2 and 5 years.