The adrenals glands are bilateral retroperitoneal organs located in the perirenal space, with an inverted V or Y morphology.
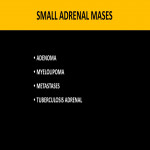
At present, with the increasing use of radiological tests, especially computed tomography (CT), there has been a significant increase in the detection of incidental adrenal lesions, known as adrenal incidentalomas. The vast majority correspond to benign lesions, predominantly adenomas and myelolipomas. However, in cancer patients the probability of metastasis is substantially increased.
The role of these imaging modalities lies in the detection and characterization of adrenal morphological alterations, making it possible to differentiate benign from malignant lesions and establish a potential diagnosis.
CT CHARACTERIZATION OF THE ADRENAL MASSES: BENIGN OR MALIGNANT?
In the presence of an adrenal mass, there are imaging findings on CT that are useful to differentiate benign from malignant lesions:
- Dough size
- Growth over time
- Morphology and homogeneity
- Calcifications
- Intracellular lipid content
- Contrast vascularization, uptake and washing pattern.
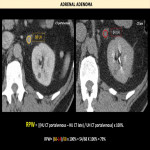
There are two criteria used on CT to differentiate benign adenomas from malignant masses: the intracellular lipid content of the mass measured in HU on non-contrast computed tomography (NCCT), and the pattern of vascular enhancement after contrast administration.
Cortical adenomas have abundant cytoplasmic fat and therefore have low attenuation in the NCCT, unlike metastases, with little intracytoplasmic fat and higher attenuation values.
In daily practice, a threshold of 10HU is used to differentiate fatty adenomas(<10HU) from other indeterminate lesions (>10HU). However, up to 30% of adenomas are low in lipids (>10UH), so we must consider another diagnostic option.
For vascular enhancement pattern evaluation, we used dynamic CT with contrast. A portal venous enhancement phase (60-80seconds post-contrast) is included to determine the percentage of contrast washout between both the initial uptake of the mass and a late phase (10-15minutes post-contrast).
The percentage of contrast washout represents the contrast portion that has washed out in the late phase concerning the contrast initially captured. The formula to calculate the percentage of relative washing (RPW) is:
- (HU CTportalvenous − HU CTlate)/(HU CTportalvenous)x 100%.
Both adenomas and metastases avidly capture contrast in the portal venous phase but differ in the RPW. Generally benign adenomas present a rapid lavage (RPW>40%) and malignant masses a slower lavage (RPW<40%).
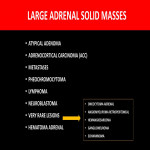
Accordingly, there are some indicative findings suggestive for malignancy: size>4cm, lesion growth, irregular borders, heterogeneous masses with cystic/necrotic/hemorrhagic components, dystrophic and irregular calcifications, punctate, and slow contrast lavage (RPW<40%). However, some lesions may present pitfalls that make their diagnosis difficult such as pheochromocytomas with micro and macroscopic fat,<10UH in NCCT, which can be misdiagnosed as adenomas.