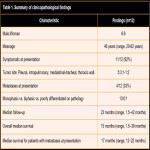
The study consisted of 6 men and 6 women. The mean age of 46 years (range, 20–62 years). Five patients had pleural SS, three had pulmonary SS, two had mediastinal SS (including one intratracheal SS), and two were present in the thoracic wall (esternal-condral and thoracoabdominal wall). The results are tabulated in Table 1.
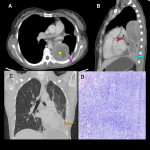
About the clinical presentation, the majority of the patients were symptomatic at presentation (11/12, 92%), with the most common presentation being dyspnea in 9/12 (75%), chest pain in 4/12 (33%), cough in 4/12 (33%), including 1 patient with hemoptysis), and a painless lump in 1/12 (8%). The remaining 1/12 (8%) patient, in spite of he was diagnosed with COVID infection, was asymptomatic but was detected incidentally on imaging. (Fig 1)
Baseline imaging of the primary was available in all the patients.
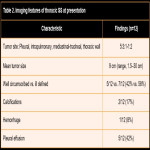
The imaging features are tabulated in Table 2.
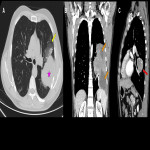
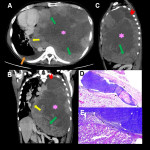
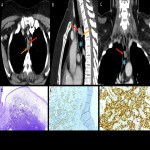
The mean size of the primary tumor on imaging was 9 cm (range, 1.5–30 cm). Margins were well circumscribed in 5/12 (42%) patients and ill-defined and infiltrative in 7/12 (58%) patients, with the ill-defined tumors having associated areas of lung atelectasis/consolidation or pleural fluid masking the tumor margins (Fig 2). Four patients had ipsilateral pleural effusion and one contralateral effusion at presentation.
On CT (n=12), all the tumors showed homogeneous solid enhancement compared to skeletal muscles. All the lesions demonstrated heterogeneous enhancement, with 11 having cystic/necrotic components. (Fig 3, 4, 5, and 6) Calcifications were present in two tumors. Hemorrhage was seen in 01 of 12 patients.
Two patients had thoracic wall tumors, with similar characteristics seen at the intrathoracic level. (Fig 7 and 8)
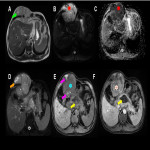
On MRI (n=1), one tumor was slightly hyperintense on T2-weighted images relative to the chest wall musculature and demonstrated low to intermediate signal intensity on T1-weighted images with T1 hyperintense hemorrhagic foci. Diffusion restriction was present in the solid portions, with heterogeneous contrast enhancement associated, predominantly peripherical. Fluid–fluid levels or ‘bowl of grapes’ appearance were not seen. (Fig 9)
One patient had a mediastinal intratracheal tumor, having a slightly heterogeneously enhancing mass without a cystic/necrotic component on CT. (Fig 10)
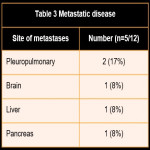
Four patients presented with metastases at the moment of diagnosis. (Table 3)
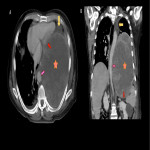
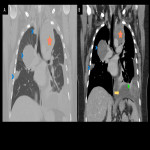
Pleuropulmonary metastases were the most common and developed in 02/12 (17%) patients and were present in the contralateral side of the primary lesion (Fig 11 and 12). Other sites of metastatic disease included the brain (1/12) (Fig 13), liver (1/12), and pancreas (1/12) (Fig 14). The remaining metastases in the liver and pancreas were present in the same patient with intrathoracic primary SS.
The metastases were either homogenous or heterogeneous with hypodense areas within. Cavitation was not present in any of the pulmonary nodules.
Pathological correlation showed that 10 patients had monophasic tumors, and 01 had a poorly differentiated tumor. There is no biphasic tumor.
The primary tumor was resected in 01 patient (tracheal SS). Ten patients received adjuvant therapy (either chemotherapy or a combination of chemotherapy and radiation), while two did not receive any treatment. Medical management was with ifosfamide and doxorubicin-based regimens, along with the use of second-line chemotherapy agents.
At the time of last follow-up, 8 patients are alive and 4 are deceased. Among of the 4 patients who died, 3 had metastatic disease at presentation.
The median follow-up for all the patients was 23 months (range, 1.5–42 months). The median survival time for all the patients was 15 months (range, 1.5–39 months), while it was 17 months for patients with metastasis at presentation (range, 12–22 months).
The limitations of our study include the retrospective analysis. Statistical analysis was not performed due to the small number of patients.