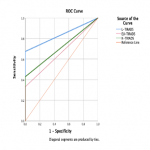
176 patients with 187 nodules, from which 151 female and 25 male were included in the study. 135 nodules (72.19%) were benign, 7 nodules (3.74%) were suspicious of malignancy, 17 nodules (9.09%) were malignant, and 14 nodules (7.49%) were non-diagnostic cytologically according to the Bethesda system. All TIRADS systems showed high sensitivity–100%. However, L-TIRADS is more accurate (71.7%) and with a better AUC (83.7%) compared to the EU-TIRADS (ACC=41.7%; AUC=66.6%) and K-TIRADS (ACC=50.3%; AUC=71.5%) (Table 1, Figure 2).
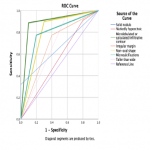
There are multiple US malignancy suggesting features, out of all microlobulated or spiculated/infiltrative contour showed high sensitivity, accuracy and AUC value – 79.2%, 85.0%, and 89.3%. As well microcalcifications showed high sensitivity and AUC value – 87.5%, 78.6% (Table 2, Figure 3).
Discussion
Among all TIRADS classifications, only the L-TIRADS AUC value was 83.7%, which is why L-TIRADS is a better Thyroid Imaging Reporting and Data System comparison to EU-TIRADS (AUC= 66.6%) and K-TIRADS (AUC=71.5%). Due to the L-TIRADS had higher AUC, specificity, and accuracy, L-TIRADS can be considered as a better system for assessing the risk of thyroid malignancy.
Based on the results of our study and the latest published studies on the comparison of malignancy-risk systems of thyroid nodules, it can be concluded that the L-TIRADS classification is of higher quality and with higher diagnostic efficiency [5, 6].
Several studies, including a study of 4,186 patients, have found a strong association between thyroid carcinoma, particularly micropapillary carcinoma, and microcalcifications in the thyroid gland (SPE 96.5%) [7]. This study cohort thyroid nodules with microcalcifications included 40 nodes (65.57%) benign, and 21 nodes malignant (34.43%), thus it can be concluded that one in three nodes with microcalcifications were malignant.
Out of the 18 nodules with a microlobulated contour, 64.3% were benign and 35.7% were malignant, as well as thyroid nodules with spiculated/infiltrative contour - 4 nodules (44.4%) were benign, and 5 nodules (55.5%) were malignant. Due to the small proportion of patients in these categories, it is not appropriate to assume these results as absolute diagnostic endpoints.
Referring to the 2018 study investigating the correlation of US malignancy features with cytopathological findings by Arpana et al., it was confirmed that several patterns such as nodule consistency, size, echogenicity, including nodule edge and contour, are important factors in distinguishing benign and malignant nodules [8].